Crit Care:克拉霉素对脓毒症、呼吸和多器官功能障碍综合征患者的影响
2022-06-21 MedSci原创 MedSci原创
克拉霉素并不能降低伴有呼吸和多器官功能障碍的脓毒症患者的死亡率。克拉霉素治疗与较低的败血症复发相关,可能通过免疫恢复机制发挥效应。
克拉霉素可能作为免疫调节治疗脓毒症和急性呼吸功能障碍综合征。然而,临床证据仍不确定。
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员的目的是评估克拉霉素是否能改善脓毒症、呼吸和多器官功能障碍综合征患者的28天死亡率。

研究人员对脓毒症患者进行了一项多中心随机临床试验。在2017年12月至2019年9月期间,研究人员招募了氧分压与吸入氧分数之比小于200且SOFA分数超过3分的参与者。患者随机接受1g克拉霉素或安慰剂静脉注射,每日1次,连续治疗4天。该研究的主要终点是28天全因死亡率,次要结局是90天死亡率、脓毒症反应(定义为SOFA评分在第7天至少降低25%)、脓毒症复发、外周血细胞数量和白细胞转录组学的差异。
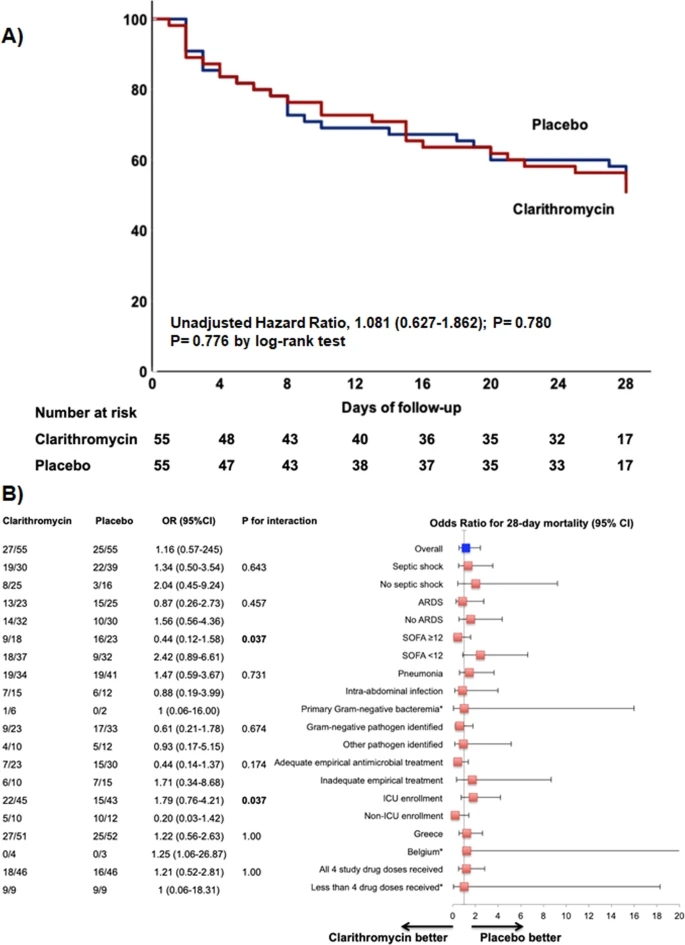
55名患者被分配到每组。到第28天,克拉霉素组有27例(49.1%)患者死亡,安慰剂组有25例(45.5%)患者死亡(风险差异为3.6%[95%可信区间(CI)为15.7-22.7];P=0.703,调整后OR为1.03[95%CI为0.35-3.06];P=0.959)。90天死亡率和脓毒症反应无统计学差异。克拉霉素治疗与较低的脓毒症复发发生率相关(OR为0.21[95%CI为0.06-0.68];P=0.012);单核细胞HLA-DR表达显著增加;非经典单核细胞扩张;且与胆固醇稳态有关的基因上调。严重和非严重不良事件分布均匀。
由此可见,克拉霉素并不能降低伴有呼吸和多器官功能障碍的脓毒症患者的死亡率。克拉霉素治疗与较低的败血症复发相关,可能通过免疫恢复机制发挥效应。
原始出处:
Eleni Karakike,et al.Effect of intravenous clarithromycin in patients with sepsis, respiratory and multiple organ dysfunction syndrome: a randomized clinical trial.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-04055-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多器官功能障碍综合征#
82
#多器官功能障碍#
94
非常不错的论文
69
非常强
82
#功能障碍#
81
#综合征#
0
#期刊论坛##学习#
80
不错的文章
67