Hypertension:急性心肌梗死后高血压、微血管病变与预后
2018-07-17 xing.T MedSci原创
由此可见,严重的进行性微血管损伤参与了高血压和急性心肌梗塞病史患者的病理生理学和预后。
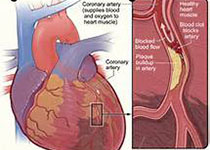
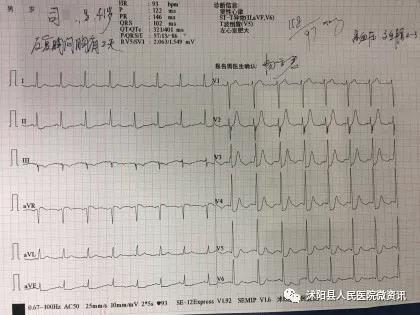
近日,心血管权威杂志Hypertension上发表了一篇研究文章,该研究的主要目的是探究急性ST段抬高心肌梗死患者与高血压病史相关的微血管损伤的病理生理学机制。
研究人员使用侵入性和非侵入性微血管损伤指标、2天和6个月的心脏磁共振成像进行了一项队列研究,并评估了长期的健康结局。
340例急性心肌梗死患者(平均年龄为59[12]岁;血压为135[25]/79[14]mmHg;男性占237人[73%],先天性高血压占105人[32%])在紧急经皮冠状动脉介入治疗期间进行了前瞻性研究。与既往没有高血压的患者相比,高血压患者年龄较大(63 [12]岁 vs. 57 [11]岁; P<0.001),吸烟者比例较低(52 [50%] vs. 144 [66%]; P=0.007)。冠状动脉血流、罪犯动脉内的微血管阻力、梗塞病变、炎症(C-反应蛋白和白细胞介素-6)与高血压无关。与既往没有高血压的患者相比,高血压患者在基线6个月时左心室射血分数改善较少(5.3[8.2]% vs. 7.4 [7.6]%; P=0.040)。出院后(中位随访4年),既往高血压是心肌梗死后2天心肌出血(1.81 [0.98-3.34]; P = 0.059)和全因死亡或心力衰竭(n=47次事件,n=24伴有高血压; 2.53[1.28-4.98]; P=0.007)存在多变量相关。
由此可见,严重的进行性微血管损伤参与了高血压和急性心肌梗塞病史患者的病理生理学和预后。
原始出处:
David Carrick,et al. Hypertension, Microvascular Pathology, and Prognosis After an Acute Myocardial Infarction.Hypertension.2018. https://doi.org/10.1161/HYPERTENSIONAHA.117.10786
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TENS#
81
#PE#
66
#血管病#
101
#微血管#
77
#血管病变#
81
#微血管病变#
87
#Hypertension#
85