CCR:干细胞加速罕见癌症治疗药物筛选
2016-08-05 佚名 生物谷
最近来自美国约翰斯霍普金斯Kimmel癌症中心的研究人员利用人类干细胞开发出一个药物筛选新系统,可能会加速对罕见癌症治疗药物的筛选过程。 相关研究发表在国际学术期刊Clinical Cancer Research上。 在这篇文章中研究人员详细描述了他们如何将人类干细胞转变为一种侵袭性罕见儿童脑癌——成神经管细胞瘤。随后再将这些癌细胞的遗传信息与成百上千种已经用于药物筛选的常见人类癌细胞进行

最近来自美国约翰斯霍普金斯Kimmel癌症中心的研究人员利用人类干细胞开发出一个药物筛选新系统,可能会加速对罕见癌症治疗药物的筛选过程。
相关研究发表在国际学术期刊Clinical Cancer Research上。
在这篇文章中研究人员详细描述了他们如何将人类干细胞转变为一种侵袭性罕见儿童脑癌——成神经管细胞瘤。随后再将这些癌细胞的遗传信息与成百上千种已经用于药物筛选的常见人类癌细胞进行对比。
研究人员表示,在构建的人类成神经管细胞瘤的细胞模型中进行筛选,进而发现癌细胞对药物的应答情况,这样可能与真实情况更具可比性。
目前儿童成神经管细胞瘤的标准治疗方法结合了放射治疗和化疗,但是其中一种叫做Group3成神经管细胞瘤的亚型容易出现复发,病人的生存率只有30%~40%。
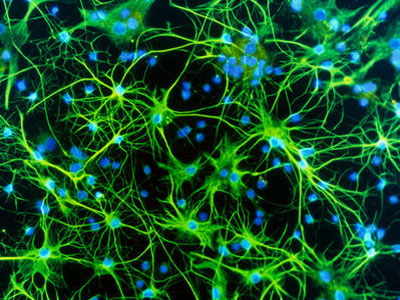
在这项研究中,科学家们使用慢病毒作为转运系统将Group 3成神经管细胞瘤中常见的癌症相关基因插入到人类神经干细胞中。随着干细胞复制,癌症相关基因能够将干细胞转变为癌细胞。这些癌细胞形成的肿瘤与真正的人类成神经管细胞瘤存在非常相似的生物学特征,其基因表达谱与人类肿瘤细胞非常吻合。
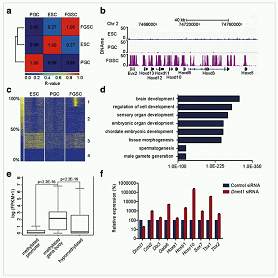
随后研究人员利用从新生的肿瘤中获得的RNA样品找到了这种类型肿瘤的基因表达特征,他们可以将这种基因表达特征在三个大型细胞系数据库中与其他细胞进行对比,这些数据库中的细胞系已经经过药物筛选,能够与现有药物进行匹配。“我们想知道我们获得的细胞是否与任何一种现有的基因表达特征相匹配。一旦两者匹配,我们就能知道哪些类型的药物更有可能杀死这些细胞。而不需要辛辛苦苦进行筛选,比如在10万种化合物中检测哪种化合物能够杀死我们获得的癌细胞。”研究人员解释道。
利用这种方法,科学家们发现一组叫做CDK抑制剂的化合物可能有望用于Group3成神经管细胞瘤的治疗。
其中一种叫做palbociclib的药物已经得到美国FDA的批准用于治疗晚期乳腺癌。当他们把这种药物加入到他们利用干细胞得到的癌细胞中,他们发现这种药物不仅能够抑制细胞生长,导致细胞凋亡增加,还能够延长肿瘤移植小鼠模型的生存时间。
研究人员表示palbociclib及其他同类药物目前已经用于儿童脑瘤的1期临床试验,他们认为该系统可能是找到治疗罕见癌症的一种新方法。
原始出处
Allison R. Hanaford, Tenley C. Archer, Antoinette Price, Ulf D. Kahlert, Jarek Maciaczyk, Guido Nikkhah, Jong Wook Kim, Tobias Ehrenberger, Paul A. Clemons, Vlado Dančík, Brinton Seashore-Ludlow, Vasanthi Viswanathan, Michelle L. Stewart, Matthew G. Rees, Alykhan Shamji, Stuart Schreiber, Ernest Fraenkel, Scott L. Pomeroy, Jill P. Mesirov, Pablo Tamayo, Charles G. Eberhart, Eric H. Raabe.DiSCoVERing Innovative Therapies for Rare Tumors: Combining Genetically Accurate Disease Models with In Silico Analysis to Identify Novel Therapeutic Targets.CCR.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,谢谢作者分享!
115
#药物筛选#
143
#治疗药物#
62
#癌症治疗#
97
#罕见#
90
#筛选#
64