患者1
【一般资料】
男,68岁
【主诉】
因上腹不适0.5d、呕血3h入院;
【体格检查】
入院时血红蛋白144g/L,入院后3h再次出现呕血1次,量约1000ml,伴大汗、心悸、头晕,血压87/58mmHg,中度贫血貌,
【辅助检查】
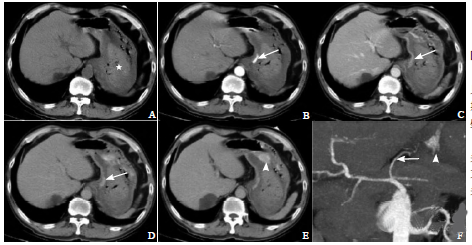
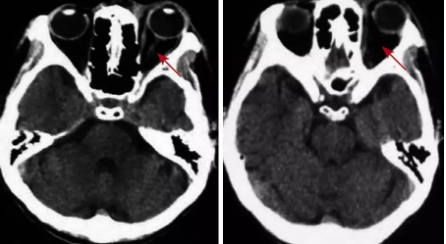
血红蛋白92g/L。CT检查见图1。急诊数字减影血管造影(DSA)检查证实:胃左动脉破裂出血,见大量对比剂外溢至胃腔内
【治疗】
遂行出血动脉栓塞,止血满意。
患者2
【一般资料】
女,77岁
【主诉】
右下肢肌间静脉血栓形成
【治疗】
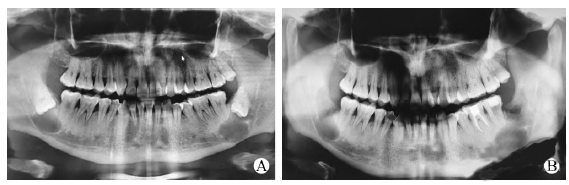
给予低分子肝素5000U皮下注射抗凝治疗,2次/d,于入院第3天清晨排干硬大便后出现便血,复查血常规:血红蛋白117g/L,较入院时下降;CT检查见图2。MSCT考虑直肠前壁活动出血;外科肛门镜直视下证实,距肛缘约5cm、直肠前壁黏膜纵行裂口,长约1cm,活动出血,行直肠黏膜破裂出血缝合止血,止血满意,术后未再出血。最后诊断直肠前壁撕裂伴活动性出血。

【讨论】
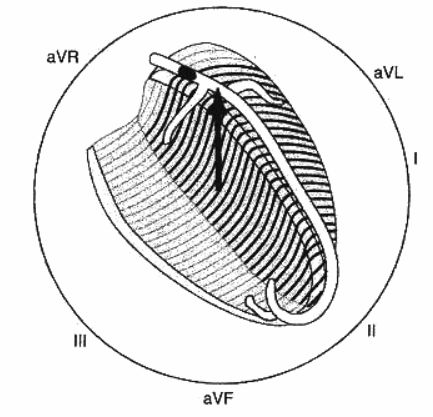
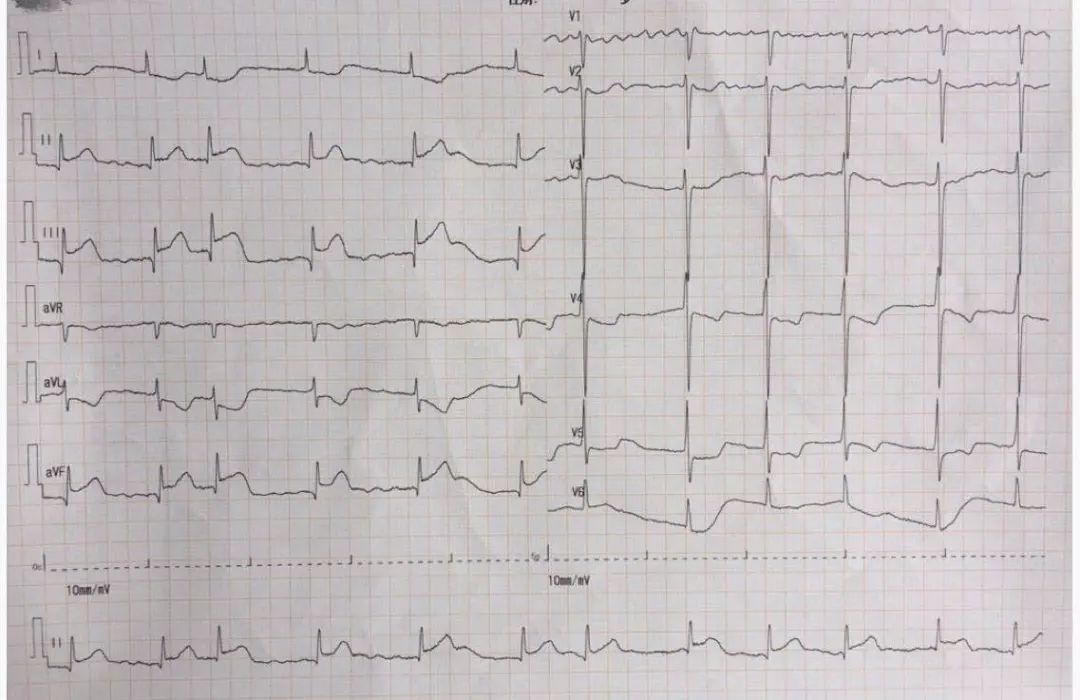
MSCT一站式急性消化道出血检查是集全腹常规平扫和多期相动态增强扫描及腹部血管重建为一体的检查方法。本研究通过实践发现,急性消化道出血的MSCT一站式检查,检查前无需进行特殊的胃肠道准备,不额外增加患者的痛苦,可即时检查,对于血流动力学不稳定的急性消化道出血患者,在积极抗休克、扩充血容量治疗的同时即可完成检查,检查方法简单,扫描时相对规范,检查时间短,检查野无盲区,可同时显示肠腔、肠壁、肠壁外及腹腔情况,图像便于观察,能满足临床急会诊需求,不仅能提供消化道腔内出血及定位的相关信息,而且能提供一系列管壁及管腔外的信息(血管畸形、消化道肿瘤等),为进一步明确出血原因提供有效证据。活动性出血在增强CT上表现为肠壁下肠腔内高密度“碘征”,即高密度的对比剂外溢至肠腔内,在动脉期即出现,随时间推移外溢对比剂剂量增加,与肠道液体混合后密度较前降低,在肠道内具有流动性和聚集性,具有特征性;藉此可与肠道内高密度食物、各种高密度外源性引入物、肠道内富血供病变、肠黏膜异常强化、患者呼吸运动及肠道蠕动产生的高密度伪影相鉴别。Sun等对113例活动性消化道出血患者进行前瞻性研究发现,MSCT血管造影诊断活动性消化道出血的敏感度和特异度分别为86.0%和100.0%;Kuhle等[5]使用单螺旋CT通过动物实验表明,当消化道活动性出血达到0.3ml/min时,CT即可检测出来,小于DSA可明确诊断0.4~0.5ml/min消化道活动性出血的量。动脉期CT扫描及血管重建可提供消化道血管解剖信息,血管解剖变异及畸形对于进一步介入治疗也具有重要意义。尽管多项研究指出MSCT诊断活动性消化道出血,其阴性预测值不如阳性预测值,但本研究结果提示,MSCT急性消化道出血检查阴性时,无需再行DSA检查[1,4,8];因此,尽管MSCT一站式急性消化道出血检查不像消化道内镜及血管造影具有治疗价值,但是检查价值是肯定的,可作为传统内镜检查的有力补充,特别是对于血流动力学不稳定的患者,能大大减少检查前的准备时间,为临床选择针对性的治疗赢得更多的时间,可推荐作为此类急性消化道出血患者的首要检查手段。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








这种探索方式很好
104
#消化道#
55
#CT表现#
68
学习了.涨知识了!
101
学习了.谢谢分享.
0