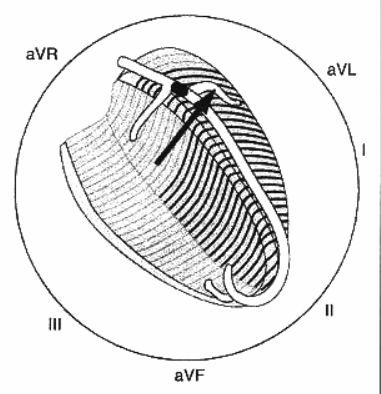
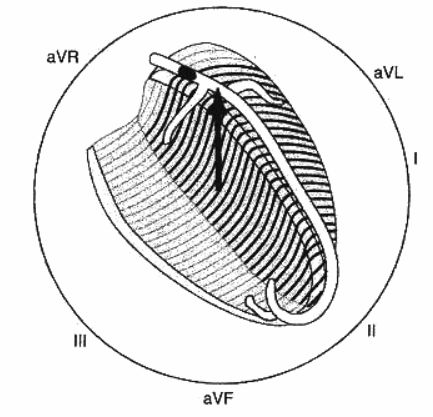
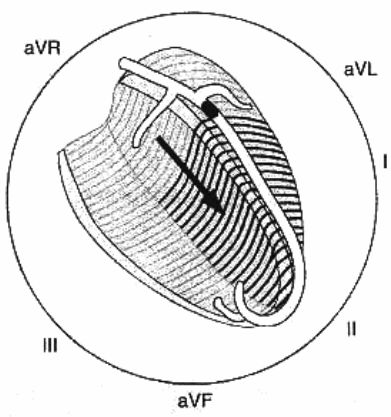
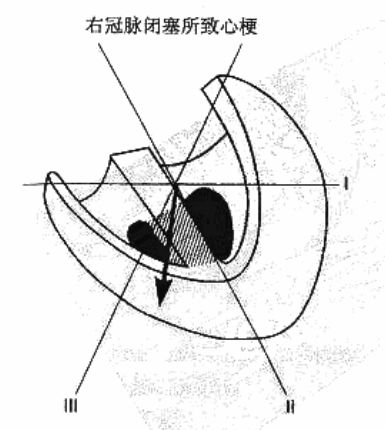
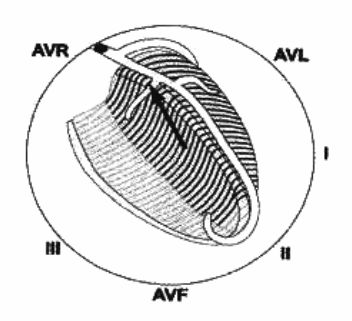
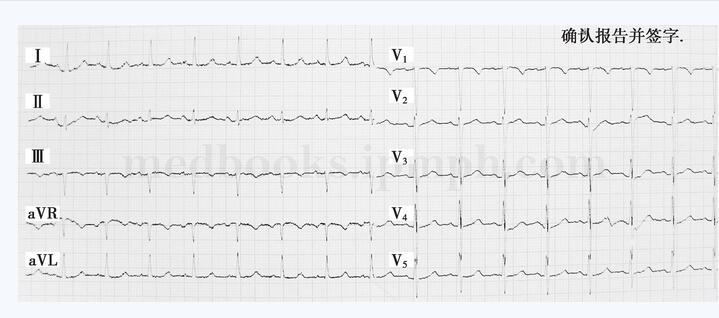
7张图教你判断急性ST段抬高型心梗闭塞部位
2018-01-15 王加伟 医学界心血管频道
急诊心电图明确提示是急性ST段抬高型心梗,当我们快速说出其中可能发生急性闭塞的罪犯血管时,急诊医生总会问起:你是如何根据心电图判断出急性ST段抬高型心梗罪犯血管的呢?



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ST段抬高型心梗#
94
学习一下很不错
104
学习了谢谢分享!!
107
收藏起来.谢谢分享!
89
学习了谢谢分享!!
105
#ST段抬高#
58
#ST段#
69
好的教学材料
89
学习了很有用不错
50