肿瘤疫苗+PD1,黑色素瘤患者完全缓解率45%!获得FDA突破性疗法认定
2020-12-17 医药魔方 医药魔方
12月15日,IO Biotech公司宣布FDA授予其开发的肿瘤疫苗IO102和IO103联合抗PD-1单抗治疗不可切除/转移性黑素瘤突破性疗法资格。
12月15日,IO Biotech公司宣布FDA授予其开发的肿瘤疫苗IO102和IO103联合抗PD-1单抗治疗不可切除/转移性黑素瘤突破性疗法资格。
一项代号为MM1636的I/II期临床研究共纳入30例转移性黑色素瘤患者,患者接受纳武利尤单抗联合肿瘤疫苗IO102和IO103作为一线治疗。患者每2周接受1次纳武利尤单抗治疗,每2周注射一次IO102和IO103,注射6次IO102和IO103之后,变为4周给予一次,直至一年。然后评估该联合疗法的安全性、血液和活检中的免疫反应以及疗效。 中位随访时间为15个月,有1例患者正在等待评估,29例患者疗效可评估,总体缓解率(ORR)达79%,PD-L1阳性和阴性患者的ORR分别为94%和62%。数据截止期,45%的患者得到完全缓解,34%的患者得到部分缓解,数值明显高于丹麦转移性黑色素瘤数据库提取的PD-1单药标准疗法对照数据。
中位无进展生存期(mPFS)为25.6个月。除了疫苗接种部位局部反应外,联合疗法的毒性与纳武利尤单抗单药治疗相当。所有接受治疗患者外周血单核细胞(PBMC)和肿瘤部位均可检测到针对IDO和/或PD-L1的疫苗特异性T细胞。
IO102和 IO103是IO公司基于其T-win?技术平台开发的first-in-class免疫调节疫苗,能够参与并激活IDO和PD-L1特异性人类T细胞,从而具有双重作用机制,既可以靶向和直接杀死免疫抑制细胞和肿瘤细胞,同时可以间接激活其他T效应细胞,产生强大的抗肿瘤活性。
黑色素瘤是黑色素细胞来源的一种高度恶性的肿瘤,多发生于皮肤,也可见于黏膜、内脏、眼底,或原发病灶不明。全球每年有大约20万人被诊断为黑色素瘤,白种人黑色素瘤90%属于非肢端皮肤型,中国人群则以黏膜和肢端皮肤型为主。与其他实体瘤相比,黑色素瘤除早期手术切除外,缺乏特效治疗,预后差,致死年龄更低。
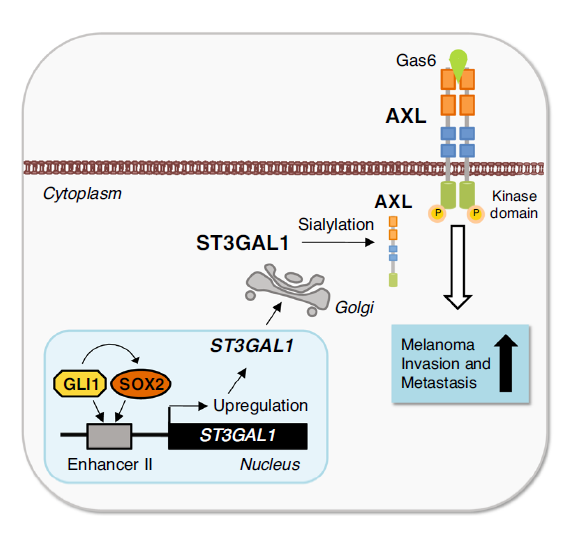
大多数黑色素瘤存在MAPK信号通路激活,如BRAF、NRAS、NF1突变,其中NRAS激活突变占15%~25%,BRAF激活突变占40%-60%,达拉非尼+曲美替尼、维莫非尼等药物的获批上市也为黑色素瘤提供了一个口服靶向组合疗法。此外,黑色素瘤通常被认为是免疫原性最高的实体瘤,因此对免疫疗法高度敏感,Keytruda、Opdivo等PD1单抗药物最先获批的适应症也均为黑色素瘤,为BRAF抑制剂耐药的患者提供了二线治疗的新选择。但是当晚期黑色素瘤患者对PD1药物也发生耐药之后,就面临无药可用的局面。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#完全缓解#
74
#色素#
68
#突破性疗法#
88
#黑色素#
71
#黑色素#
64