Radiology:在判断肺癌浸润性时,每个影像科医生都该认识的征象!
2021-07-22 shaosai MedSci原创
肺癌占全球所有癌症相关死亡的四分之一,其中肺癌最常见的组织学亚型为肺腺癌。根据多学科分类对肺腺癌的侵袭性进行评价,该分类包括原位癌(AIS)、微浸润性腺癌(MIA)和浸润性腺癌(IVA)。
 肺癌占全球所有癌症相关死亡的四分之一,其中肺癌最常见的组织学亚型为肺腺癌。根据多学科分类对肺腺癌的侵袭性进行评价,该分类包括原位癌(AIS)、微浸润性腺癌(MIA)和浸润性腺癌(IVA)。由于诊断决定了治疗过程进而影响预后,因此肺癌的浸润程度与患者生存显著相关。CT是临床上诊断肺癌的常规影像学手段。因此,提高CT诊断肺癌浸润程度的准确性将为肺癌患者提供更多的临床益处。
肺癌占全球所有癌症相关死亡的四分之一,其中肺癌最常见的组织学亚型为肺腺癌。根据多学科分类对肺腺癌的侵袭性进行评价,该分类包括原位癌(AIS)、微浸润性腺癌(MIA)和浸润性腺癌(IVA)。由于诊断决定了治疗过程进而影响预后,因此肺癌的浸润程度与患者生存显著相关。CT是临床上诊断肺癌的常规影像学手段。因此,提高CT诊断肺癌浸润程度的准确性将为肺癌患者提供更多的临床益处。
自2017年以来投入临床使用的高空间分辨率(HSR)CT扫描仪,其空间分辨率高达150毫米。由于对技术特性的进一步改进,例如探测器大小、焦点尺寸和X射线管,HSR CT在平面内和人体轴位方向上均具有极高的的分辨率,可为临床提供精细的肺部解剖结构和病变的详细信息。据我们所知,现阶段尚无评估HSR CT在临床实践中诊断肺癌性能的相关研究。
近日,发表在Radiology杂志的一项研究探讨来HSR CT在预测肺腺癌侵袭性方面的诊断价值,为HSR CT在肺癌诊断的进一步应用铺平了道路,为临床早期、准确的诊断肺癌浸润程度提供技术支持。
本项回顾性研究纳入了在2018年1月至2019年12月期间因肺癌接受手术的原位腺癌(AIS)、微浸润腺癌(MIA)或浸润性腺癌(IVA)的连续89例患者。所有患者均行HSR CT扫描,层厚为0.25 mm,矩阵为2048。由两位独立的阅读者对HSR CT表现进行了评估:有无分叶征、毛刺征、胸膜凹陷、血管集束、均匀的磨玻璃样影、网状影、不规则和中心性实性成分、空气支气管征(不规则、截断或扩张)。对结节的总直径(≤1.6 cm或>1.6 cm)和实性部分的最长径(≤0.8 cm或>0.8 cm)进行评估。使用Logistic回归模型来确定与MIA + IVA相关的特征。对受试者工作特性对诊断性能进行分析。
本研究共对89例患者(平均69岁±11岁[标准差];49名男性)进行了评估。浸润性结节的大小平均为2.5 cm±1.2。单因素分析显示分叶征、毛刺征、胸膜凹陷、不规则和中央性实性成分、空气支气管征、总直径和实性部分直径与MIA及IVA相关(P均 < 0.05)。在校正年龄、性别和吸烟包年后,空气支气管征和实性成分直径大于0.8 cm仍然是预测浸润性的独立因子(P = .001和P = .02)。这两项结果的组合诊断性能如下:敏感性97%(61例患者中的59例;95%置信区间:94%,100%),特异性为86%(22例患者中有19例;95%置信区间:65%,97%),曲线下面积为0.94。
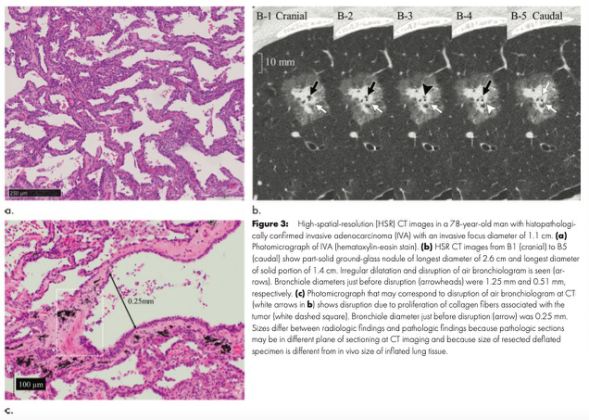
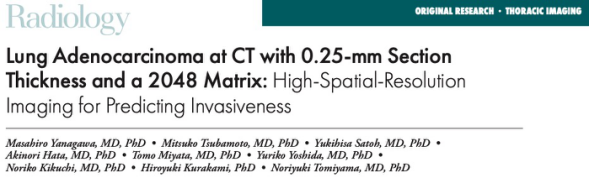
图1 78岁男性,病理学证实为浸润性腺癌(IVA)的高空间分辨率(HSR) CT图像,浸润性病灶直径为1.1 cm。(a) IVA的显微照片(苏木精-伊红染色)。(b) B1(头)至B5(尾部)HSR CT图像显示亚实性磨玻璃结节,直径2.6 cm,实性部分最长直径1.4 cm。图中可见不规则的支气管扩张和截断(箭头)。细支气管截断前的直径(箭头)分别为1.25 mm和0.51 mm。(c)与CT上支气管的截断相对应的可能显微照片(b中的白色箭头)显示,肿瘤相关的胶原纤维增生造成支气管的破坏(白色虚线方框)。细支气管截断前的直径(箭头)为0.25 mm。
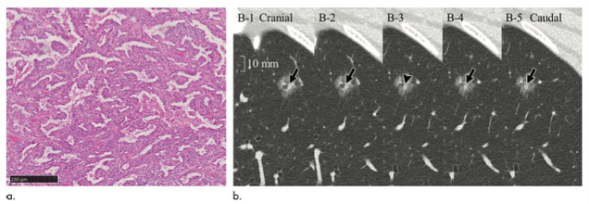
图2 59岁女性,病理证实为微创腺癌(MIA)的高空间分辨率(HSR) CT图像,浸润性病灶直径为0.4 cm。(a) MIA的显微照片(苏木精-伊红染色)。(b) B1(头)至B5(尾部)HSR CT图像显示亚实性磨玻璃结节直径1.5 cm,实性部分直径0.5 cm。可见支气管不规则的轻度扩张和截断(箭头)。细支气管截断前的直径(箭头所示)为0.81 mm。
图3 77岁男性,病理证实为腺癌原位(AIS)的高空间分辨率(HSR) CT图像。(a, b)AIS显微照片显示间质纤维化,但无浸润病灶。(c) C1(头)至C5(尾部)HSR CT显示亚实性磨玻璃结节,直径1.6 cm,实性部分最长直径0.3 cm。可见支气管轻度不规则扩张,但支气管未见截断(箭头)。细支气管直径(箭头)为0.72 mm。
综上所述,两种高空间分辨率CT表现(支气管截断和实性成分的直径大于0.8 cm)可以作为预测肺腺癌侵袭性的独立预测指标。其中,支气管截断是高空间分辨率CT的一个独特征象,其对肺腺癌侵袭性的预测具有最佳的诊断效果。本研究为临床术前早期预测肺腺癌侵袭性以及预测患者预后提供了参考依据和技术支持。
原文出处:
Masahiro Yanagawa,Mitsuko Tsubamoto,Yukihisa Satoh,et al.Lung Adenocarcinoma at CT with 0.25-mm Section Thickness and a 2048 Matrix: High-Spatial-Resolution Imaging for Predicting Invasiveness.DOI:10.1148/radiol.2020201911
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#影像科#
79
学习
86
学习
88
MIA
88
学习学习
84