盘点:Nature杂志8月亮点研究看过来!
2015-08-28 佚名 生物谷
时间定格在8月底,不知不觉又到了亮点研究盘点的时间,本期小编为大家带来8月份Nature杂志众多亮点研究盘点。【1】埃博拉病毒造成的新疫情 当前由埃博拉病毒所造成的疫情正在西非蔓延。在7月22日之前的一个星期,国际卫生组织报告说,在几内亚有22个已证实的病例,在塞拉利昂有4个,在利比里亚没有——5月9日该疫情在利比里亚已宣告“结束”。本期Nature杂志的特写文章总结了在应对本次疫情中

时间定格在8月底,不知不觉又到了亮点研究盘点的时间,本期小编为大家带来8月份Nature杂志众多亮点研究盘点。
【1】埃博拉病毒造成的新疫情
当前由埃博拉病毒所造成的疫情正在西非蔓延。在7月22日之前的一个星期,国际卫生组织报告说,在几内亚有22个已证实的病例,在塞拉利昂有4个,在利比里亚没有——5月9日该疫情在利比里亚已宣告“结束”。本期Nature杂志的特写文章总结了在应对本次疫情中获得的经验教训,并对这种疾病和其他疾病在将来可以怎样得到控制表达了意见。
能量在细胞内是怎样分布的?在骨骼肌中,能量分布曾被认为是通过由代谢物促进的扩散发生的,尽管遗传证据对这种分布方式的重要性提出了疑问。Robert Balaban及同事利用各种形式的高分辨率显微镜,对线粒体本身除了实际上产生能量外是否也在其分布中起一定作用进行了研究。他们发现,通过以“质子动力”(proton-motive force)的形式在整个细胞中形成一个导电通道,它们的确在能量分布中起一定作用。在整个这一网络中,线粒体蛋白定位似乎是在变化的,从而使得线粒体膜电势能够以最佳方式产生和被利用。这一能量分布网络(它取决于传导而不是扩散)速度有可能极快,从而使得肌肉能够对新的能量需求几乎即时做出反应。
“G蛋白耦合受体”(GPCRs)是充当一系列细胞外信号的传感器的膜蛋白。它们通过“异三聚G蛋白” (能结合鸟嘌呤核苷酸的蛋白,充当细胞内分子开关)发挥功能,以变构方式将后者激活来触发GDP释放。有数百种人类GPCRs作用于16种不同的 “Gα蛋白”之上。在这篇“分析”文章中,Madan Babu及同事试图弄清是否存在一个主管Gα激活的普遍性变构机制。他们发现的确有这样一个机制:不同GPCRs 通过一个高度保守的机制与Gα蛋白发生相互作用并将其激活,这也许可解释为什么GPCR–Gα系统发生了迅速分化、同时又保留了其变构性质。
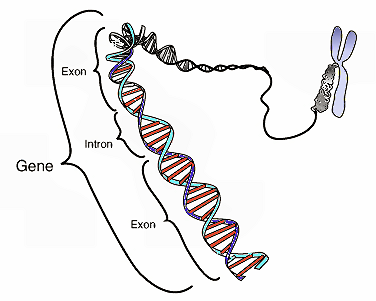
【4】小细胞肺癌的遗传原因
对110个小细胞肺癌病例所做的全基因组测序,显示了几乎所有病例中肿瘤抑制因子基因TP53和RB1的一个典型的双等位基因失活现象。在TP53 和RB1没有发生改变的仅有的两个样本中,“染色体碎裂”(chromothripsis)将 “cyclin D1”激活,导致同样的分子效应。另外,25%的肿瘤在NOTCH家族的基因中携带能造成失活的突变,同时作者也发现,一个临床前小鼠模型中Notch信号作用的激活可以降低肿瘤数量和延长突变小鼠的生存时间。这项研究突显了作为最具致命性的人类癌症之一的这种肺癌的可能的药物作用目标。
【5】让金属玻璃恢复“青春”
当一个玻璃系统慢慢向平衡态放松时,我们就说它在 “老化”,其很多材料性质会发生相应变化。通过能量注入使该系统从平衡态又回到原来的状态(比如说通过加热它或以机械方式对其施压),就可以使它恢复“青春”。现在,Sergey Ketov等人发现,这样的青春焕发可以在要温和很多的条件下做到。仅仅通过在一个远远低于玻璃转变温度的温度下对玻璃(在本例中采用金属玻璃)进行热循环,就可以在很大程度上让其恢复青春。作者将这一现象归因于玻璃态中内在结构异质性的效应,这种异质性随着温度的变化会转变成局部化的内应变,不同区域会发生不同程度的膨胀和收缩。
【6】新的肝细胞
新的肝细胞作为体内平衡程序的一部分是怎样在成年肝脏中出现的仍不清楚。Roel Nusse及同事利用复杂细胞标记方法对这一问题进行了研究。他们在中央静脉附近识别出一类增殖的肝细胞,它们是双倍体(相比之下成熟细胞是多倍体),表达一个肝脏祖细胞标记。这些细胞对由来自中央静脉的相邻内皮细胞提供的Wnt信号做出反应,成为能够取代维持肝脏平衡所需的所有肝细胞类型的多倍体肝细胞。
包括胰腺导管腺癌(PDA)在内的各种不同癌症已知取决于高水平的自噬过程,它是正常细胞中营养清除和质量控制活动所需的高度保守的自行降解过程。在这项研究中,Rushika Perera等人描述了细胞压力和自噬过程之间在胰腺癌中导致细胞代谢被改变的一个以前人们不知道的联系。他们发现,MiT/TFE家族转录因子的异常表达和组成性激发,通过人类PDA标本和细胞系中大大增强的自噬-溶酶体功能介导代谢重新编程。这些发现说明,溶酶体调控是癌细胞中营养利用和能量平衡的一个焦点。
这项研究描述了“缺氧诱导因子”(HIF)异二聚体、包括与小分子和DNA相结合的复合物的等待已久的晶体结构。HIFs是协调细胞对低氧压力的适应性的转录因子,是癌症治疗的潜在目标。小鼠的HIF–ARNT异二聚体被发现有一个与含bHLH-PAS的生物钟成分CLOCK–BMAL1截然不同的架构。与癌症相关的HIF-α 突变可以被映射到重要的结构区域,这些结构在未来可以为小分子药物发现工作提供参考。
【9】μ-阿片受体的激发
μ-阿片受体是被各种止痛药、内源性内啡肽和被滥用的药物如海洛因和鸦片激发的一种“G-蛋白耦合受体”。我们对激动剂的结合导致某一特定的G-蛋白子类被识别、耦合和激发的机制还不完全了解。在本期Nature上的两篇论文中,作者采用X-射线晶体学方法、分子动态模拟方法和NMR光谱方法对受体激发的结构基础进行了研究。除了揭示这一GPCR在细胞外和细胞内区域中所发生的与受体激发相关的构形变化外,这两项研究也可帮助解释为什么这一受体的激动剂结合穴与胞质G-蛋白耦合界面之间的变构耦合相对较弱。
【10】营养: 更好地认识儿童营养不良
Nature Communications上发表的一篇论文描述了环境性肠病(EE,这种病被广泛认为是造成儿童营养不良的一个重要原因)的一个潜在病因。作者建立了这种病的第一个动物模型,发现了饮食和微生物共同作用来改变小鼠小肠、以产生类似于人类EE病症状的证据。
营养不良是一个重要的全球性健康问题,在五岁以下儿童的全部死亡病例中占20%。EE是小肠的一种慢性炎症,人们对其病因很不了解,有些人还认为它是造成营养不良儿童的治疗干预措施成功率低(不到三分之一)的原因。另外,也不存在这种疾病的动物模型,所以除了试验潜在治疗药物有困难外,了解其病因和发展也一直有困难。
现在,Brett Finlay及同事建立了这种疾病的一个小鼠模型,发现让小鼠幼崽吃一种中度营养不足的饮食,同时让其口腔反复接触与粪便相关的细菌(也就是重现比较差的卫生条件),会诱发这些小鼠出现该疾病的症状。当本文作者再给这些小鼠幼崽喂食一种正常饮食21一天时间时,它们的生长平均被抑制30%,同时还表现出蛋白吸收方面的问题以及小肠渗透性的提高。这些发现表明,营养不足的饮食改变了小肠的生态系统,并允许从环境获得的微生物定植。还有必要做进一步的研究来确定小鼠这种效应的精确机制并弄清这是否也适用于患EE的儿童。
本周发表在《科学报告》上的两则研究报道了温度的变化对于北京死亡率和广州减寿年数的影响。这两项研究都表明在较极端温度下,需要加强防护措施。
在第一项研究中,李湉湉和她的研究团队使用气候变化预测的每日平均气温的增加来估算心血管疾病和呼吸疾病会出现的潜在死亡数字。他们的分析显示,按照政府间气候变化专门委员会(Intergovernmental Panel on Climate Change,IPCC)的RCP4.5情景(该情景中温室气体排放量在2040年会达到顶峰,然后下降),和上世纪80年代相比,2020年代、2050年代、2080年代北京由心血管疾病导致的死亡每年会增加529人,734人和844人(数字为中位数)。研究者的分析也显示呼吸疾病导致的死亡在2020年代、2050年代、2080年代每年会增加155,216和248人。而如果温室气体排放遵循了RCP8.5的情景,也就是21世纪排放不断增加的话,增加的死亡人数会更多。
在另一项研究当中,刘起勇和他的研究团队分析了2003年到2007年期间广州居民受到寒冷天气和炎热天气的影响产生的减寿年数。减寿年数(Year of Life Lost, YLL)考虑进了在死亡时间的语气寿命,给年轻人的死亡权重更重。他们的分析表明,在广州,寒冷的环境温度比炎热的对于减寿年数的影响比炎热的更强。研究者表示,炎热温度对于减寿年数的影响是立即的,并且只持续4天,而寒冷温度对于减寿年数的影响是延迟的,但是可以持续14天左右。研究者表示,无论是炎热还是寒冷的天气,75岁以下和受教育程度低的人都更容易受到影响。
本期Nature Communications上发表的一篇论文报告说,在快速眼动(REM)睡眠期间的人脑活动与在清醒注视期间所观察到的脑活动非常相似。这项研究也许可解释为什么从REM睡眠状态清醒过来的人经常会谈到鲜活的梦境。
在REM睡眠期间,我们眼睛的转动方式与我们处于清醒状态、在看某一视觉场景时的转动方式非常像。科学家早就想弄清REM是否反映了睡眠期间的视觉信息处理方式。
Yuval Nir及同事记录了19个人的脑活动。他们发现,当患者在睡眠期间、清醒期间、以及在视觉刺激场景期间发生快速眼动时,其大脑的内侧颞叶(对长期记忆形成有重要作用的一个脑区域)中的各个神经元会以相似方式做出反应。这说明,睡眠期间的快速眼动相应于类似视觉的信息的处理期间,可能的确反映了做梦过程中的视觉表象。
【13】癌症: 磁场为杀手细胞指路
Nature Communications上发表的一项研究报告说,临床磁共振成像(MRI)系统在小鼠中可被用来将能够杀灭癌症的细胞向肿瘤引导,并抑制它们的生长。这些发现表明,由MRI系统产生的磁场能够以特定细胞为目标来用于治疗。
MRI扫描仪(通常用在医院里)利用强磁场来生成高分辨率解剖图像,这种图像可用来定位身体中的肿瘤。Munnita Muthana、Aneurin Kennerley及同事获取了携带选择性感染和杀死肿瘤细胞的一种病毒的小鼠免疫细胞,让它们吸收氧化铁纳米颗粒。这些磁化的免疫细胞然后被注射到有前列腺肿瘤的小鼠体内。通过利用一台MRI扫描仪来生成脉冲化的磁场梯度,该小组然后将能够杀灭癌症的细胞向前列腺癌或已经扩散到肺部的癌症引导,所产生的整体效应是前列腺肿瘤的生长受到了抑制。
虽然现有的临床MRI扫描仪有可能产生这样的磁场,但目前还不清楚这种方法对人类是否也会有效。
本期Nature Communications上发表的一项研究描述了治疗阿尔茨海默氏症的一个新的潜在方法。这项研究显示,通过以在调控身体免疫系统中起重要作用的特定白细胞(被称为调控性T-细胞)为治疗目标,阿尔茨海默氏症的关键症状在小鼠身上可以得到成功治疗。
阿尔茨海默氏症影响中枢神经系统,导致神经损伤、被称为斑块的蛋白块形成和慢性炎症。以前人们已经意识到,当将免疫细胞朝向中枢神经系统引导时,这些症状会减轻。
在这篇论文中,Michal Schwartz及同事显示,阻断特定T-细胞(被称为Foxp3+ Tregs)的活性,可以使更多免疫细胞超小鼠脑运动。因此,炎症和斑块会减少,实验鼠在认知试验中表现会更好。这项研究显示了调控性T-细胞在影响大脑的疾病中所起的一个作用。它也表明,这些细胞是未来治疗阿尔茨海默氏症的可能药物目标。
【15】地球科学: 物种大灭绝的一个前兆
本期Nature Communications发表了畸形浮游生物可能指示物种大灭绝其他驱动因素的证据。虽然冰川事件以前曾被与最古老的重大物种灭绝联系起来,但作者提出,造成物种大灭绝的原因更有可能是海洋中缺氧现象和有害金属的大范围存在。
奥陶纪-志留纪灭绝事件被认为是在距今4.2亿年前以脉冲形式出现的,当时绝大多数生命都在海洋中,陆地上存活下来的非常少。以前的研究表明,这些事件是气候变冷和生境减少造成的,但那些模型并不能解释所有古生物学和地球化学观察结果。
Thijs Vandenbroucke及同事发现,晚志留纪一次灭绝事件开始期间发生的浮游生物畸形是与现代生物对当今高含量的金属毒物的反应非常相似的方式发生的。作者提出,金属中毒还可能造成了远古时代的畸形现象,因为畸形浮游生物与它们在其中被保留下来的岩石中金属含量的急剧增加在时间上是巧合的。高含量的金属表明当时的海洋化学环境发生了变化,也表明缺氧的大范围存在可能是这些早期灭绝事件期间造成生物被杀死的一个机制。
最近的研究工作表明缺氧在海洋中是物种大灭绝背后的一个驱动力量,这项研究支持这一观点,并且表明畸形浮游生物化石也许是识别这些低氧时期开始时间的一个新的“法医学”工具。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
55
这篇文章有一定深度
151
是一篇不错的文章
151
棒
148
我喜欢
160
免疫和阿尔茨海默病
167
好好
82
好好
74