A&R:Notch-1在高安动脉炎患者MTOR过度活跃和血管炎症中的关键作用
2022-07-28 MedSci原创 MedSci原创
来自Takayasu动脉炎(TA)患者的CD4+ T细胞中Notch-1的表达升高,导致mTORC1过度活跃和促炎T细胞分化。靶向Notch-1是TA临床管理的一种有前途的治疗策略。
目的:Takayasu动脉炎(TA)是一种主要影响主动脉和主要分支的慢性和进行性自身免疫性大血管血管炎,特征是血管层存在进行性炎症。在来自苏州大学最近的研究中,研究团队确定了雷帕霉素机制靶标(mTOR)过度活跃在TA中促炎T细胞分化中的核心作用。本研究旨在探索支持T细胞内在mTOR过度活跃和 TA血管炎症的潜在机制,重点是Notch-1。
方法:根据Notch-1、活化的Notch-1和HES-1水平确定Notch-1的表达和活性。研究人员通过测量细胞内磷酸化核糖体蛋白S6表达的方法来检测mTOR活性。通过检测Th1和Th17谱系决定转录因子来分析促炎T 细胞的分化。使用γ-分泌酶抑制剂DAPT和使用短发夹RNA (shRNA)策略的基因敲低评估Notch-1的功能。使用人源化NSG小鼠嵌合体进行转化研究,使用来自TA患者的免疫细胞诱导了人类血管炎。
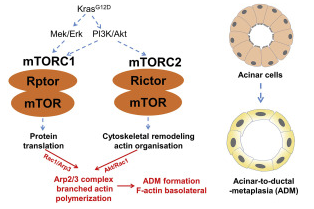
结果:来自TA患者的CD4+ T细胞高表达Notch-1,并导致mTOR过度活跃和Th1 细胞和Th17细胞的自发分化不良。使用DAPT和Notch-1 shRNA阻断Notch-1有效地消除了 mTOR 复合物1 (mTORC1)激活和促炎T细胞分化。机制上,Notch-1促进mTOR表达,与mTOR相互作用,并与mTOR的溶酶体定位相关。因此,DAPT和CD4+ T细胞特异性基因敲除Notch-1的全身给药可以减轻人源化TA嵌合体的血管炎症。
结论:来自TA患者的CD4+ T细胞中Notch-1的表达升高,导致mTORC1过度活跃和促炎T细胞分化。靶向Notch-1是TA临床管理的一种有前途的治疗策略。
出处:Jiang W, Sun M, Wang Y, et al. Critical Role of Notch-1 in Mechanistic Target of Rapamycin Hyperactivity and Vascular Inflammation in Patients With Takayasu Arteritis. Arthritis Rheumatol. 2022 Jul;74(7):1235-1244. doi: 10.1002/art.42103. Epub 2022 Jun 2. PMID: 35212196.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Notch-1#
83
#动脉炎#
0
#中的关键作用#
106
#过度活跃#
92
#血管炎#
139
#Notch#
102
#血管炎症#
86
#OTC#
85