女24岁 “尿失禁”竟24年
2017-08-03 那彦群 陈 山 泌尿外科疑难病例讨论精选
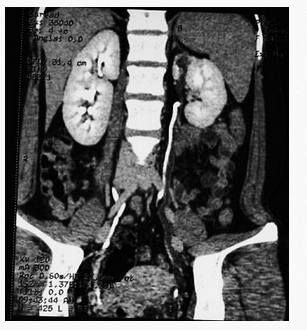
女性患者24岁,“尿失禁”24年,发现右侧双肾盂双输尿管畸形1个月。如何进行治疗?【病例资料】患者女性,24岁。主诉:“尿失禁”24年,发现右侧双肾盂双输尿管畸形1个月。现病史:患者自出生起开始出现溢尿,立位、卧位均出现,每日溢尿总量约为300~400ml,同时患者可正常排尿,有膀胱憋尿感,一直未予治疗。自述发病以来无明显疼痛不适、尿路刺激、血尿等症状。2008年3月20日患者曾就诊于我院妇产




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了谢谢分享
91
学习了,谢谢分享
84
#尿失禁#
52
好好学习下吧
85
学习了谢谢分享
88
学习了谢谢分享
85
学习谢谢分享
0
学习学习学习
47
不错的文章不错的文章
48
总结本例患者的诊治经过,我们有以下几点体会:①尿瘘患者必须行膀胱镜及妇科(女性患者)检查明确病因;②重复肾畸形多半双侧,对一侧明确的要考虑对侧的诊断进行B超、IVU、CTU、MRU等检查明确肾脏位置及发育情况;③手术前必须明确异位开口位置,如IVU或CTU不能明确位置,须通过瘘口插入输尿管导管或穿刺造影检查;④患侧肾发育不良且伴有漏尿可行异位肾及输尿管切除术,若重复肾功能良好,可予异位开口之畸形输尿管离断并输尿管膀胱再植术。
44