Eur Heart J:MI后接受DAPT的患者采用PPI治疗可使胃肠道出血风险降低
2019-03-10 xing.T 网络
由此可见,质子泵抑制剂治疗的使用程度低于MI后接受DAPT治疗的指南原则,并且通常与降低UGI出血风险有关。考虑到总体出血风险较低,应更多地关注确定从PPI治疗中获益最多的患者。
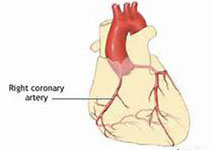
对于接受双重抗血小板治疗(DAPT)治疗的患者,他们对预防胃肠道出血的治疗建议有所不同。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员试图分析质子泵抑制剂(PPIs)预防DAPT治疗的心肌梗死(MI)患者上胃肠道(UGI)出血的有效性,这与当前的欧洲心脏病学会指南建议相关。
研究人员链接到丹麦全国登记处,以确定出院后7天因急性心肌梗死而接受DAPT治疗的患者,并将抗生素治疗的患者排除在外。研究人员使用多重Cox回归建模来计算与PPI使用相关的UGI出血的平均风险。根据指南风险评估比较相关的治疗效果。
研究人员分析46301例心肌梗死后接受DAPT治疗的患者。根据指南标准,只有35%的UGI出血风险较高的患者接受了PPI治疗。对于高危患者,1年的UGI出血风险为1.0%[95%可信区间(CI)为0.9-1.1%]和1.7%(CI为1.5-2.0%)。与未治疗相比,总体PPI与UGI出血风险比为0.62(CI为0.48-0.77),相对应的绝对风险差异为0.44%(CI为0.39-0.48%)。对于高危患者,质子泵抑制剂治疗与类似的绝对风险差异相关[0.47%(CI为0.43-0.51%)]。
由此可见,质子泵抑制剂治疗的使用程度低于MI后接受DAPT治疗的指南原则,并且通常与降低UGI出血风险有关。考虑到总体出血风险较低,应更多地关注确定从PPI治疗中获益最多的患者。
原始出处:
Thomas S G Sehested.et al.Reduced risk of gastrointestinal bleeding associated with proton pump inhibitor therapy in patients treated with dual antiplatelet therapy after myocardial infarction.Eur Heart J.https://doi.org/10.1093/eurheartj/ehz104
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险降低#
51
#胃肠道#
54
#ART#
63
#DAPT#
60
#胃肠道出血#
72
#HEART#
47