J Clin Oncol:CMB305联合阿特珠单抗治疗局部晚期滑膜肉瘤或粘液样脂肪肉瘤患者的疗效和安全性
2021-07-20 MedSci原创 MedSci原创
CMB305联合阿特珠单抗治疗局部晚期滑膜肉瘤或粘液样脂肪肉瘤患者的疗效和安全性
癌症的治疗性疫苗接种应可诱导有效的、稳定的、且能自我更新的T细胞,能够直接靶向特定的肿瘤相关抗原。CMB305 是一种异源的初免-加强疫苗接种方案,用于对 NY-ESO-1 特异性 CD8 T 细胞群进行初免,然后用有效的 TLR-4 激动剂激活免疫反应。
这是一项开放标签的随机2期试验,旨在评估CMB305方案联合阿特珠单抗与单用阿特珠单抗相比用于滑膜肉瘤或粘液样脂肪肉瘤患者的疗效和安全性。
Sant P. Chawla, et al. Phase II Randomized Study of CMB305 and Atezolizumab Compared With Atezolizumab Alone in Soft-Tissue Sarcomas Expressing NY-ESO-1. Journal of Clinical Oncology
招募了局部晚期、复发或转移的滑膜肉瘤或粘液样脂肪肉瘤患者,随机分成了两组,分别接受CMB305联合阿特珠单抗(实验组)或单纯阿特珠单抗(对照组)治疗。主要终点是无进展生存期(PFS)和总生存期(OS)。同时还评估了安全性和免疫反应。
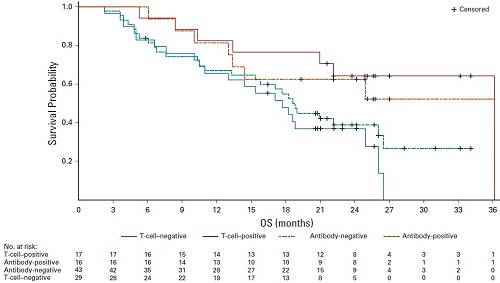
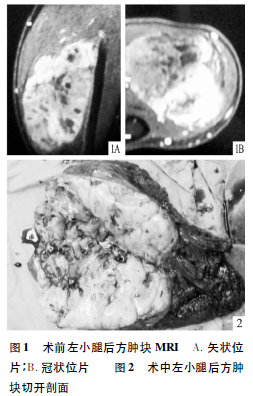
两组的PFS和OS
共招募了89位患者;55.1%的患者既往至少接受了2线化疗。联合组和对照组的中位PFS分别是2.6个月和1.6个月(风险比[HR] 0.9,95%CI 0.60-1.3)。两组的中位OS都是18个月。接受联合治疗的患者的治疗诱导的NY-ESO-1特异性T细胞率和NY-ESO-1特异性抗体反应率均显著更高(p=0.01和p<0.0001)。
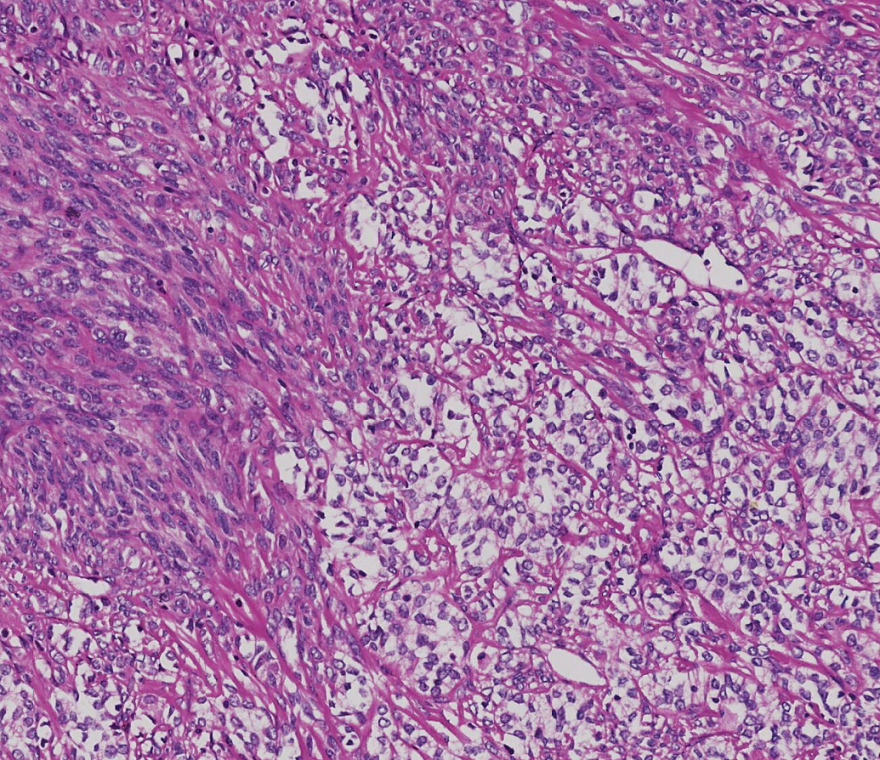
有无抗NY-ESO-1 T细胞免疫反应的患者存活预后
在对接受各种剂量的患者的事后分析中,获得了抗NY-ESO-1 T细胞免疫反应的患者亚组的OS更长(36个月;HR 0.3; p=0.02)。
综上所述,虽然与单用阿特珠单抗相比,CMB305联合阿特珠单抗未显著延长滑膜肉瘤或粘液样脂肪肉瘤患者的PFS和OS;部分患者表现出抗NY-ESO-1免疫反应的证据,并且似乎比没有这种免疫反应的患者的预后表现更好。该联合方案值得在其他临床缓解中进一步评估。
原始出处:
Sant P. Chawla, et al. Phase II Randomized Study of CMB305 and Atezolizumab Compared With Atezolizumab Alone in Soft-Tissue Sarcomas Expressing NY-ESO-1. Journal of Clinical Oncology. July 14, 2021. https://ascopubs.org/doi/full/10.1200/JCO.20.03452
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
64
#滑膜肉瘤#
64
#粘液样#
78
#疗效和安全性#
52
#局部晚期#
65
#局部#
72
谢谢梅斯提供这么好的信息,学到很多
75
谢谢梅斯分享这么多精彩信息
71
好文章
92