Blood:血小板-VWF通过刺激Tie-2防止白细胞外渗时血浆渗漏
2020-05-16 QQY MedSci原创
血小板通过与内皮VWF结合并释放Angpt1,阻止中性粒细胞穿出血管时血浆渗漏。 血小板释放的Angpt1刺激内皮细胞Tie-2,从而激活可增强皮质肌动蛋白束的GEF FGD5。
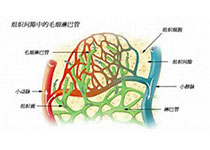
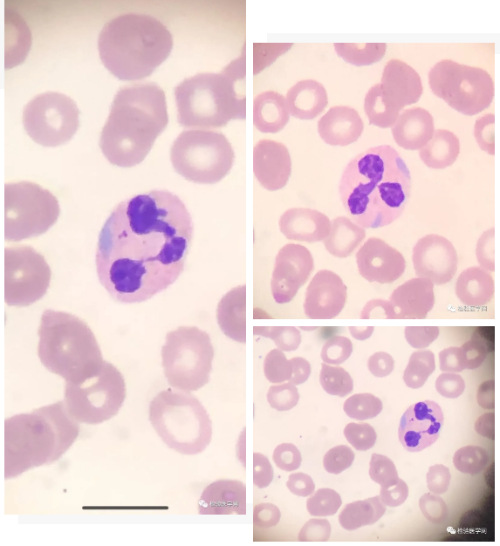
近期,Braun等明确了负责防止血浆渗漏的受体系统。研究人员通过荧光微球发现,沉默或失活内皮细胞的Tie-2都可以导致毛细血管后嗜中性粒细胞外渗部位的微静脉渗漏形成。血浆渗漏依赖于中性粒细胞外渗,因为中性粒细胞耗竭时就不存在血浆渗漏。
此外,研究人员还发现Cdc42 GTPase交换因子FGD5是Tie-2的下游靶点,在预防中性粒细胞外渗过程血浆渗漏中在发挥关键作用。在寻找Tie-2激动剂及其来源时,研究人员发现血小板源的血管生成素-1对于预防中性粒细胞引起的渗漏必不可少。
有趣的是,阻断血管性血友病因子(VWF)可导致血管在白细胞迁移过程中血浆渗漏,这表明血小板与内皮VWF之间的相互作用,可通过分泌血管生成素-1激活Tie-2,从而防止血细胞外渗诱导的血浆渗漏。
原始出处:
Laura J. Braun, et al. Platelets docking to VWF prevent leaks during leukocyte extravasation by stimulating Tie-2. Blood. May 5, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血浆渗漏#
71
#Tie-2#
64
#vWF#
57