NEJM:流感神药Xofluza上市,一粒搞定流感
2018-10-28 MedSci MedSci原创
美国FDA宣布批准由日本盐野义制药公司(Shionogi)和罗氏(Roche)联合研发的抗流感新药Xofluza(baloxavir marboxil)上市,用于治疗12岁以上无并发症的急性流感患者。这是近20年以来,FDA批准的第一款具有创新作用机制的抗流感新药。去年该药首先在日本上市,就刮起一阵旋风。上个月发表在NEJM上的研究报道称,在2期研究中,使用本药物,与安慰剂相比,流感的症状缩短23
美国FDA宣布批准由日本盐野义制药公司(Shionogi)和罗氏(Roche)联合研发的抗流感新药Xofluza(baloxavir marboxil)上市,用于治疗12岁以上无并发症的急性流感患者。这是近20年以来,FDA批准的第一款具有创新作用机制的抗流感新药。去年该药首先在日本上市,就刮起一阵旋风。今年年初,Xofluza就已经在日本获批投产和出售,值得一提的是,Xofluza只需服用一次的剂量就可在一天内治愈流感,有专家指出,Xofluza1片就能抵得上10片当下的标准疗法,且能持续起效10天,因此也被称为“最强抗流感神药”,相比之下,达菲需要每日服用两次,连服五日。
上个月发表在NEJM上的研究报道称,在2期研究中,使用本药物,与安慰剂相比,流感的症状缩短23.4-28.2小时。从2016年11月到2018年1月间招募了1494名志愿者。采取多中心、随机、双盲实验,将志愿者分为成年组、青少年组,并分别进行Xofluza、奥司他韦、安慰剂给药的3期研究。在3期研究中发现使用baloxavir平均症状缩短至53.7小时,与奥司他韦(奥司他韦75mg,一天两次,连续用5天)相似,而安慰剂组则长达80.2小时。其不良反应与安慰剂一致。另外,它还可以针对禽流感病毒H5N1和H7N9的抗Tamiflu抗性病毒株,快速杀灭病毒为可以及时阻止病毒传播,在某些次要终点中,与Tamiflu相比,它甚至表现出更强的疗效,包括停止病毒释放和降低体内病毒水平的时间。

流感是由于流感病毒感染导致的传染性呼吸道疾病。它是对公众健康的严重威胁。在世界范围内,每年有大约300-500万严重流感患者,超过100万患者需要住院接受护理,大约65万人因此去世。在流感患者患病48小时内,使用抗病毒药物可以降低疾病的症状和持续时间。
Xofluza是作为一种流感药物(5'帽状结构(CAP)依赖型核酸内切酶抑制剂),其最大的特征是仅需服用一剂,且不受年龄限制(包括儿童、青少年以及成人)。
由日本盐野义制药公司和罗氏合作研发的Xofluza是一种“first-in-class”的口服抗病毒药物,只需服用一次就可以见效。它能够治疗对奥司他韦(oseltamivir)产生抗性的病毒株和禽流感病毒株(H7N9,H5N1)。Xofluza的作用机制与目前已有抗病毒疗法不同。它通过抑制流感病毒中的cap-依赖型核酸内切酶(cap-dependent endonuclease)起到抑制病毒复制的作用。已有抗流感药物的作用机制是通过靶向神经氨酸酶(neuraminidase)。与这些药物相比,Xofluza靶向病毒复制周期的更早阶段。Xofluza在美国的新药申请获得了FDA授予的优先审评资格。
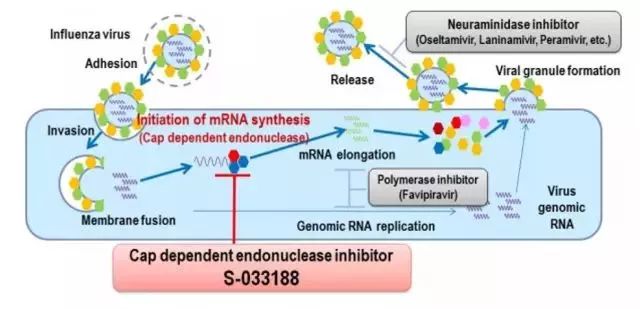
▲Xofluza作用机制(图片来源:盐野义制药公司官网)
“这是FDA近20年来批准的第一款具有创新作用机制的新抗流感疗法。每年成千上万的患者感染流感,其中很多人症状很严重,拥有安全有效的治疗选择非常重要。这款新药提供了一种重要的医疗选择。”FDA局长Scott Gottlieb博士说。
FDA药物评估和研究中心抗病毒产品部主任Debra Birnkrant博士补充道:“拥有更多使用不同机制攻击病毒的治疗选择非常重要,因为流感病毒可以对抗病毒药物产生抗性。”
我们祝愿这款新药能够在流感季节中发挥它的威力,缓解众多流感患者的症状。
参考资料:
FDA approves new drug to treat influenza. Retrieved October 24, 2018
Hayden FG, Sugaya N, Hirotsu N, Lee N, de Jong MD, Hurt AC, Ishida T, Sekino H, Yamada K, Portsmouth S, Kawaguchi K, Shishido T, Arai M, Tsuchiya K, Uehara T, Watanabe A; Baloxavir Marboxil Investigators Group.Baloxavir Marboxil for Uncomplicated Influenza in Adults and Adolescents. N Engl J Med. 2018 Sep 6;379(10):913-923
Noshi T, Kitano M, Taniguchi K, Yamamoto A, Omoto S, Baba K, Hashimoto T, Ishida K, Kushima Y, Hattori K, Kawai M, Yoshida R, Kobayashi M, Yoshinaga T, Sato A, Okamatsu M, Sakoda Y, Kida H, Shishido T, Naito A. In vitro characterization of baloxavir acid, a first-in-class cap-dependent endonuclease inhibitor of the influenza virus polymerase PA subunit. Antiviral Res. 2018 Oct 11. pii: S0166-3542(18)30363-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Xofluza#
67
学习了,谢谢分享
92
学习了
88
学习谢谢分享
85
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
97