科学家发现21种全新潜在药物靶点
2017-09-04 佚名 新浪
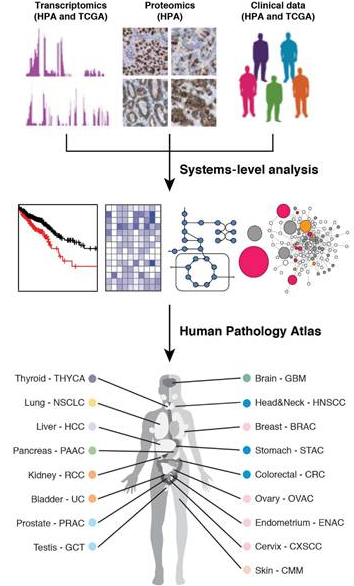
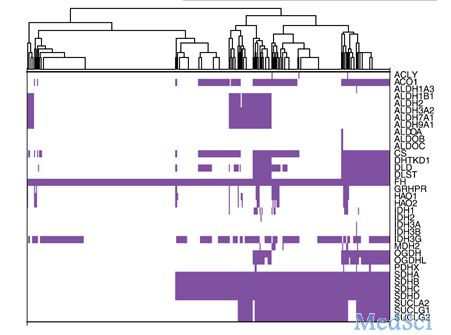
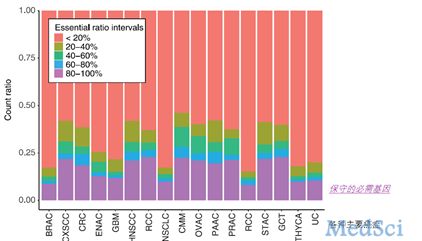
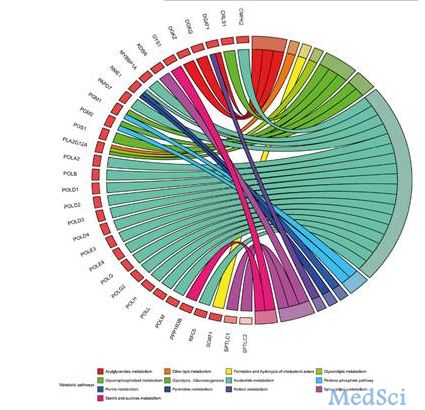
来自瑞典的科学家在8月的《科学》杂志上发表文章,通过对9,666人的基因测序的研究,分析17种癌症的转录组学、蛋白质组学和临床数据,得到了人类癌症病理学图集。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#潜在药物#
67
#科学家发现#
49
#药物靶点#
0
学习了谢谢分享
0
不一定是每一个target都有临床应用价值
79