消化道大出血诊治中有哪些应注意的问题?临床医生速点开
2019-02-25 张筱凤 中华医学信息导报
消化道短时间内大量出血称急性大出血,并伴有血容量减少引起的急性周围循环障碍。
消化道短时间内大量出血称急性大出血,并伴有血容量减少引起的急性周围循环障碍。临床上,出血量超过1000 ml的急性大量失血,进展迅猛,病情变化快,短时间内即可出现失血性休克,常出乎医务人员的意料,造成患者不良损害结果及预后,是引发消化内科医疗纠纷的重要原因之一。本文旨在通过典型案例的简析,进而扩展总结消化道大出血诊治中的过错防范建议,以指导临床工作,尽量减少医疗纠纷的发生。
案例回顾
患者,男,50岁,因“黑便、呕血一天”于XXXX年2月20日至A医院急诊,以消化道出血收住入院,入院时查体:体温37.3℃,血压70/50 mmHg (1 mmHg =0.133 kPa),神清,气平,两肺呼吸音粗,未闻及杂音。全腹软,无压痛,无反跳痛,肝脾肋下未及,肠鸣音5次/min。双下肢无浮肿。入院后诊断:上消化道出血(肝硬化?食道胃底静脉曲张破裂出血?失血性休克)。予告病危,降门静脉压、抑酸止血、抗感染及备血等处理。当日查血红蛋白88 g/L,肝功能γ-谷氨酰转肽酶125 U/L(参考值0~53 U/L),白蛋白31 g/L(参考值35~55 g/L),总蛋白54 g/L。
2月21日9时,入院后患者未出现呕血,解黑便200 ml。复查大便隐血试验 阳性,血红蛋白73 g/L。当晚19时10分患者体温38.6℃。予安乃近退热治疗。 2月22日10时患者体温38.5℃。予以冰枕物理降温。18时45分,患者呕血2次, 量约500 ml,含血凝块,解暗红色血便1次,量约200 ml。查体:血压70/40 mmHg,心率130次/min。予扩容、止血、输血及降低门脉压力等治疗。邀外科和ICU科会诊。21时3分患者出现神志不清,无呼吸。予气管插管、胸外心脏按压等抢救措施。21时13分床旁彩超检查提示:右肝钙化灶,肝区回声增 粗,胆囊内壁胆固醇结晶。经抢救至22时,患者血压、心跳、脉搏未恢复,大动脉搏动消失,双侧瞳孔散大固定,心电图示一直线,宣告临床死亡。
诊疗解析
处理消化道大出血的基本原则之一是针对病因迅速止血。上消化道出血常见的病因是消化性溃疡、食管胃底静脉曲张破裂、急性糜烂性出血性胃炎和胃癌。其中,食管胃底静脉曲张破裂出血,来势凶猛,出血量大,并发症多,再出血率高,预后不良,死亡率极高,尤其需要及早检查明确诊断。
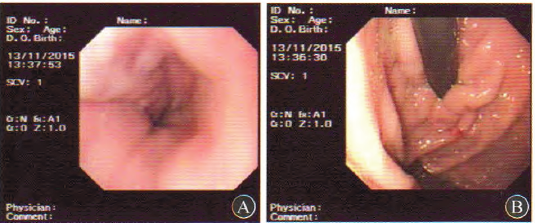
胃镜检查是目前诊断上消化道出血病因的首选方法,诊断正确率达80%~94%,可解决90%以上消化道出血的病因诊断。一般主张胃镜检查在出血后12~48 h内进行,也称急诊胃镜检查,可提高出血病因诊断的准确性。急诊胃镜检查还可以根据病变的特征判断是否继续出血或估计再出血的危险性,并同时进行内镜止血治疗。当内镜下有下列表现之一时,静脉曲张出血的诊断即可成立:曲张静脉的急性出血(喷射性出血或渗血);曲张静脉表面有“血栓头”;曲张静脉表面覆有血凝块;出血的食管胃底静脉曲张患者未发现其他潜在的出血部位。
本案例中,医院在患者呕血、解柏油样便,并出现失血性休克系列症状后,将其收住入院、诊断及救治措施正确,但在患者病情相对稳定时,尤其临床已考虑肝硬化、食管胃底静脉曲张破裂出血时,胃镜及其他检查欠及时,未能最终明确消化道出血原因。
消化道大出血诊治中的过错防范建议
上述案例提示,对于消化道大出血患者,尽早明确出血原因和出血部位是救治成功的关键。除此之外,还需对病史采集、密切观察生命体征、综合救治等予以高度重视。为了减少消化道大出血诊治过程中医疗纠纷的发生,医务人员应在以下几方面予以注意:
1.重视病史采集及必要的检查:认真了解患者的病史,实验室检查、影像学检查及查体情况,结合患者个体情况认真分析消化道出血的风险程度,将其危害性、应对措施以及本院的条件限制等作为重要内容告知患方。
2.密切观察生命体征,正确评估出血量及是否还有活动性出血:消化道出血病情严重度与失血量呈正相关,因呕血与黑便混有胃内容物与粪便,而部分血液贮留在胃肠道内未排出,故难以根据呕血或黑便量判断出血量。临床上应根据综合指标判断失血量,如根据血容量减少导致周围循环的改变(伴随症状、心率和血压、实验室检查)来判断失血量;休克指数(心率/收缩压)是判断失血量的重要指标;体格检查中可以通过皮肤黏膜色泽、颈静脉充盈程度、意识和尿量等情况来判断血容量减少程度;客观指标包括中心静脉压和血乳酸水平。
同时应严密观察病情,判断是否还存在活动性出血,有以下情况者要考虑到仍有活动性出血:①呕血或黑便次数增多,呕吐物呈鲜红色或排出暗红血便,或伴有肠鸣音活跃;②经快速输液输血,周围循环衰竭的表现未见明显改善,或虽暂时好转而又再恶化,中心静脉压仍有波动,稍稳定又再下降,红细胞计数、血红蛋白浓度与红细胞压积继续下降,网织红细胞计数持续增高;③补液与尿量足够的情况下,血尿素氮持续或再次增高。
3.综合救治,积极补充血容量,快速纠正休克:在发现消化道大出血合并失血性休克时,应立即组织救治,必要时请上级医师到场指导,并请麻醉科、ICU、血液科等相关科室共同参与。在给氧、建立两条以上静脉通道及安置尿管的基础上开展抗休克综合治疗,及时输血,快速补充足够血容量。出血量较大时,需要尽早输血。如果有凝血功能障碍,需要输新鲜血或血小板。血压不能稳定时需要使用血管活性药。综合救治要有条不紊,密切合作。
4.积极查找出血原因,实施可靠的止血措施:对怀疑或已经诊断上消化道出血的患者,在迅速稳定其生命体征的基础上应争取急诊胃镜检查,以明确出血原因并进行内镜下止血。临床对反复消化道大出血患者,应尽早行急诊内镜检查以明确出血部位及性质,对初次内镜检查阴性者,要重视复查内镜检查。对考虑小肠大出血患者,在条件允许的情况下,建议先急诊行小肠CT检查,再进行选择性血管造影检查。对出血量不大或大出血经治疗病情稳定者,也应尽早先行小肠CT检查,再选择胶囊内镜检查,根据小肠CT或胶囊内镜结果来选择单气囊或双气囊电子小肠镜检查。
药物联合内镜治疗是目前治疗急性上消化道出血的主要方法,可明显提高止血成功率。对于食管胃底静脉曲张出血患者,可根据医院条件、医师经验和患者病情综合考虑,选择内镜下曲张静脉套扎术、硬化剂或组织黏合剂注射治疗。非静脉曲张性出血常用的内镜止血方法包括药物局部注射、热凝止血和机械止血,药物注射治疗联合热凝或机械止血方法可以进一步提高局部病灶的止血效果。药物治疗方面,对因消化性溃疡、急性胃黏膜损害、食管贲门黏膜撕裂症、门脉高压性胃病等非静脉曲张所致的出血首选应用质子泵抑制剂,对肝硬化食管胃底静脉曲张破裂出血首选应用垂体后叶素或生长抑素等降低门静脉压力的药物。
5.高度重视消化道出血预后不良的高危患者,及时沟通并充分告知病情:临床应早期识别再出血及死亡危险性高的患者,并予加强监护和积极治疗。提示预后不良危险性增高的主要因素有:①高龄患者;②有严重的伴随疾病(心、肺、肝、肾功能不全,脑血管意外等);③本次出血量大或短期内反复出血;④特殊病因和部位的出血(如食管胃底静脉曲张破裂出血、Dieulafoy病);⑤胃镜检查见消化性溃疡活动性出血,或近期出血征象如溃疡面上暴露血管或有血痂。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#消化道大出血#
73
好
93
#大出血#
56
#消化道#
45
#临床医生#
67
谢谢分享
87