序言
消化道出血主要表现为呕血和便血,消化道大出血常伴有低血容量性减少,出血量达到1000ml或血容量的20%可危及生命,是临床上常见的且严重的消化系统急症。
消化道是按照屈氏韧带分为上、下消化道,上消化道主要是指胃、食管、十二指肠的出血,以及胰腺、胆道的出血、胃肠吻合术后的空肠出血。
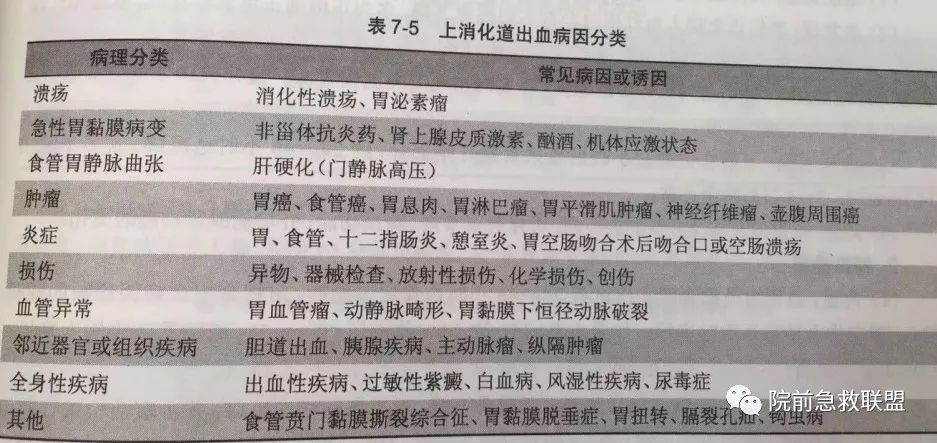
病因
上消化道最常见的病因是消化性溃疡、食管胃底静脉曲张、急性胃黏膜病变和胃癌。
临床表现
1.呕血:上消化道急性大出血常表现为为呕血,多为咖啡色胃内容物,出血速度快、量大常为暗红色或鲜红色,也可有血块,上消化道出血均有黑便,也就是柏油样大便。
2.周围循环衰竭:由于大出血,导致有效循环血量减少,从而出现周围循环衰竭,表现为头晕、乏力、心悸、晕厥、四肢发冷、面色苍白、脉速、血压下降,休克发生后出现四肢湿冷、烦躁不安、精神萎靡、呼吸急促等。
3.贫血:大量出血容易导致失血性贫血,慢性失血是贫血主要的病因,出血头晕,乏力、心悸等。
4.发热:主要是由于血容量减少、贫血、周围循环衰竭血液中的蛋白质分解吸收导致。
5.氮质血症:消化道出血导致大量血液蛋白的消化道产物在肠道吸收,引起BUN升高,从而使肾血流量减少所导致。
辅助检查
1.实验室检查
(1)隐血试验:大便或者呕吐物隐血试验强阳性是诊断消化道出血重要依据。
(2)血常规检查:急性患者出现不同程度的血红蛋白减少,呈现正细胞低色素性贫血;门静脉高压症合并脾功能亢进者,则贫血加重,白细胞及血小板进一步减少;慢性失血多是小细胞低色素性贫血,为缺铁性贫血。
(3)尿素氮检查:上消化道大量出血数小时开始升高,24~48小时达到高峰,3~4天恢复正常,可引起肠源性氮质血症。

2.急诊内镜检查
急诊内镜检查已列为急性上消化道出血的首选检查方法。急诊内镜是安全可靠的,其并发症与常规镜检并无差别;如果病情许可,镜检时间越早越好,可提高诊断的正确率。
出血征象判断
(1)失血量的评估
成人每日消化道出血5~10ml大便潜血试验阳性;
出血在50~100ml可以出现黑便;
胃内积血在250~300ml引起呕血;
出血量达到1000ml暗红色血便。
(2)活动性出血的判断
1.反复呕血或黑便稀薄且次数增加;呕血转为鲜红色,黑便呈暗红色,伴肠鸣音亢进者。
2.外周循环衰竭,经补足血容量后无明显改善或改善后又恶化;经快速补充血容量后,中心静脉压仍波动或稍稳定后又下降者。
3.血红蛋白、红细胞、红细胞压积继续下降,网织红细胞持续升高者。
4.补液及尿量足够而尿素氮持续或再升高者。
5.内镜下表现为喷血或渗血不止者。
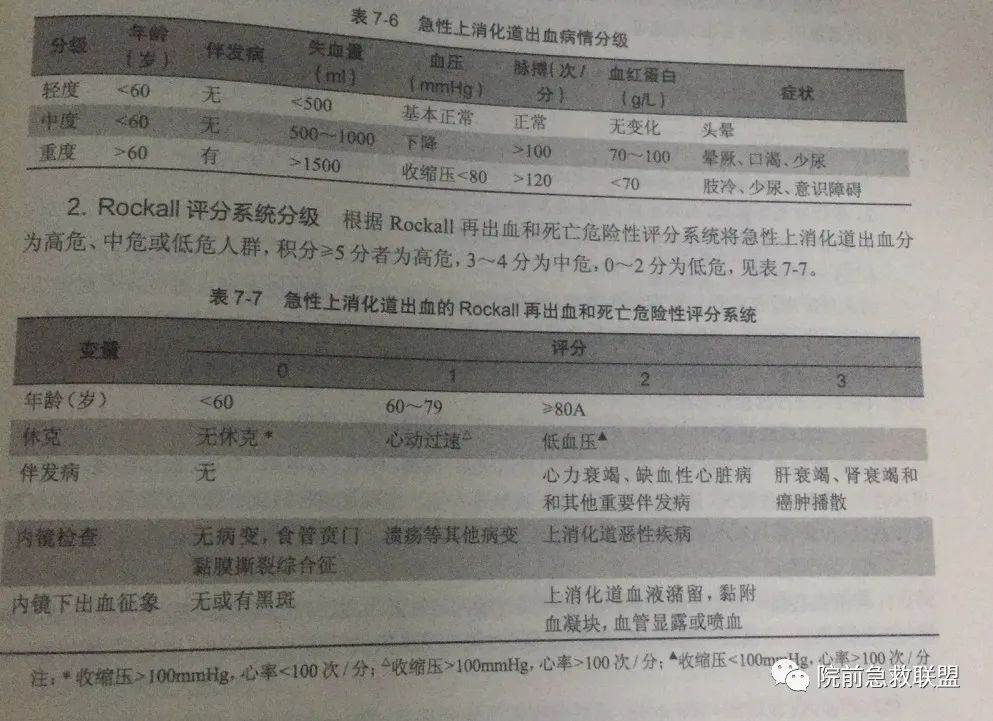
病情程度及预后分级
根据年龄,有无并发症、失血量等指标,急性消化道出血可分为轻、中、重度。
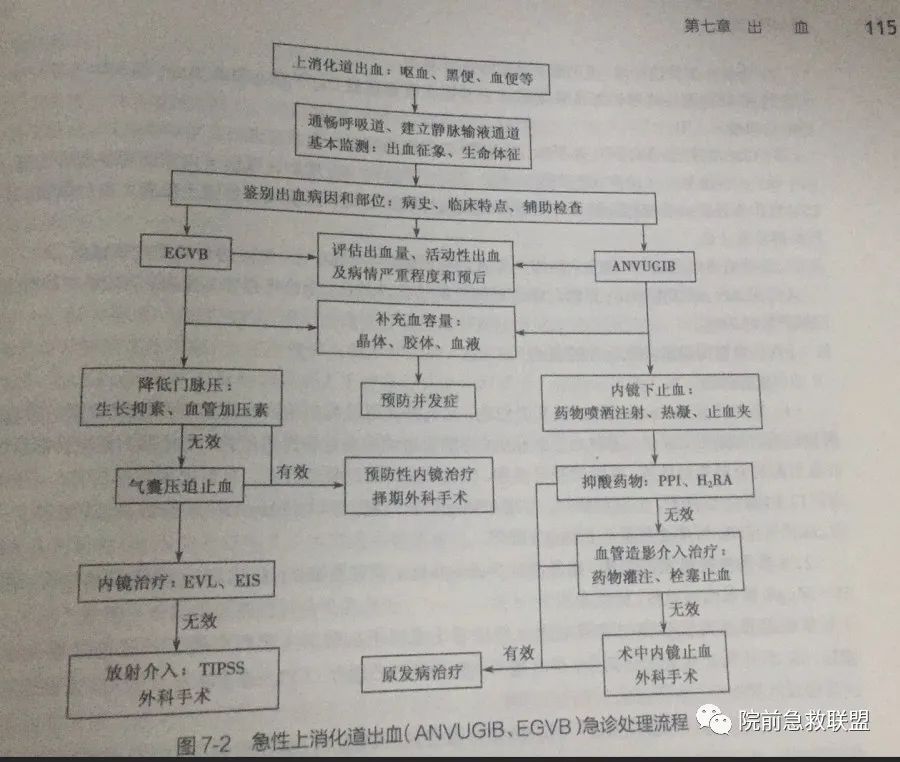
处理措施
(一)处理原则
1.判断出血征象和监测生命体征,评估出血量和活动性出血,病情的严重程度和预后。
2.积极补充血容量及止血治疗,预防并发症发生。
3.进行病因治疗,对症支持治疗。

(二)处理措施
1.现场及运送患者途中,密切观察血压、脉搏、呼吸及神志。
2.卧床休息和监测生命体征,有一点很重要,呕血的患者一定要注意头偏向一侧或者侧卧,以防呕血时导致窒息。大量出血的急性期要禁止饮食,少量出血时可以选择进食或者温良的全流食。
3.吸氧,保持安静,对烦躁不安者可给予镇静剂(肝病患者慎用)。
4.建立静脉通道,静脉输注生理盐水、葡萄糖盐水等。可用全血、血浆或生理盐水等迅速补充容量。输液速度和种类最好根据中心静脉压和每小时尿量来调节。一般认为输血的指征有:烦渴、冷汗、休克者;收缩压低于12kPa(90mmHg),脉率在120次/min以上者;血红蛋白在70g/L以下且继续出血者。
肝硬化食管胃底静脉曲张破裂出血者不宜用右旋糖酐类及不宜过多使用库血,亦不宜输液(输血)过多、过快,以免诱发肝性脑病和再出血。
5.对于反复呕吐者应放入鼻胃管或三腔二囊管压迫止血。
6.食管胃底静脉曲张破裂出血者,应禁食两三天。其他呕血者禁食4小时,如无呕血或单纯黑便者,可进食温凉流质,逐步过渡到半流质饮食。
7.内镜检查和内镜下止血。内镜检查是明确消化道出血病灶的关键检查,应在出血后24~48小时内行急诊胃镜检查,前提为生命体征平稳。内镜下有一些止血的方法,包括喷洒止血药物、热凝固止血,还可以放置血管钳去钳夹出血的血管断端。
8.药物止血。药物止血包括抑酸的药物和止血的药物。
(1)去甲肾上腺素:8mg加入100mL水中分次口服,或经过鼻胃管注入。
(2)根据出血性质选用云南白药、维生素K、安络血、凝血酶、6-氨基乙酸、抗血纤溶芳酸、酚磺乙胺等。
(3)垂体后叶素:20~40单位加入10%葡萄糖液500mL,静脉滴注(高血压病、动脉硬化、心力衰竭、肺源性心脏病、妊娠期患者禁用)。近年来采用生长抑素,可使血流减少及门脉压降低,但不伴有全身血流动力学改变。
(4)抑酸剂的应用:可选用H2-受体拮抗剂或质子泵抑制剂奥美拉唑,对控制消化性溃疡出血有效。
急性上消化道出血的处置流程
(参考文献及图片来源:第三版 急诊与灾难医学)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#上消化道#
89
>不错
0
#消化道#
106
感谢分享,学习了
69
坚持学习
87
涨知识
91