Eur Urol:盆腔淋巴结转移的预测:一项国际多中心研究
2021-06-03 AlexYang MedSci原创
在局部前列腺癌(PCa)患者中,机器人辅助前列腺根治术(RARP)已经成为最常见的治愈性手术治疗方案。扩展盆腔淋巴结清扫术(ePLND)是存在盆腔淋巴结转移(pN1疾病)分期方法的金标准,国际临床实践
在局部前列腺癌(PCa)患者中,机器人辅助前列腺根治术(RARP)已经成为最常见的治愈性手术治疗方案。扩展盆腔淋巴结清扫术(ePLND)是存在盆腔淋巴结转移(pN1疾病)分期方法的金标准,国际临床实践指南推荐用于中、高风险疾病患者。是否进行ePLND是基于成熟的术前列线图,如Briganti 2017列线图、Memorial Sloan Kettering癌症中心(MSKCC)列线图或Briganti 2019列线图。

目前有不同的列线图用于预测术前个体前列腺癌(PCa)患者的盆腔淋巴结转移性疾病情况。这些列线图没有纳入现代成像技术,如前列腺特异性膜抗原(PSMA)正电子发射断层扫描(PET)。
近期,有研究人员确定了Briganti 2017、Memorial Sloan Kettering癌症中心(MSKCC)和Briganti 2019列线图在纳入PSMA-PET后的预测性能情况。研究是在一个国际化多中心的现今队列中进行,包括了进行机器人辅助前列腺根治术(RARP)和扩展盆腔淋巴结清扫术(ePLND)的局部PCa患者。
研究包括了2016年1月至2020年11月期间在三个转诊中心进行PSMA-PET的757名合格患者,且均在RARP和ePLND手术进行。总的来说,186/757名患者(25%)在组织病理学检查中患有盆腔淋巴结转移性(pN1)疾病。Briganti 2017、MSKCC和Briganti 2019列线图的AUC分别为0.70(95%置信区间[95% CI]:0.64-0.77)、0.71(95% CI:0.65-0.77)和0.76(95% CI:0.71-0.82)。当把PSMA-PET的研究结果加入到列线图中时,发现其与pN1疾病有明显的关联(p<0.001)。PSMA-PET的加入大大改善了模型的鉴别能力,三种列线图的交叉验证AUC分别为0.76(95% CI:0.70-0.82)、0.77(95% CI:0.72-0.83)和0.82(95% CI:0.76-0.87)。在决策曲线分析中,将PSMA-PET加入到三个列线图中能够增加净收益。
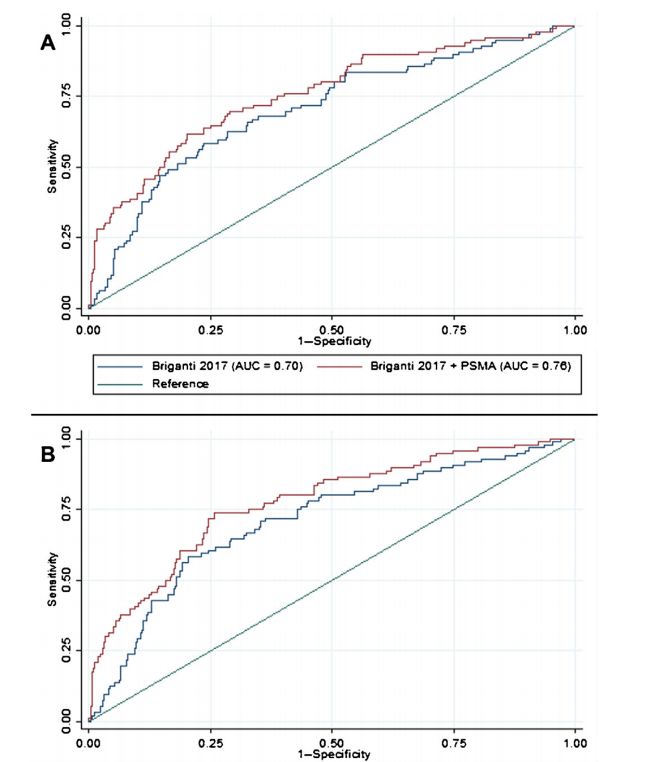

三种列线图的ROC曲线分析
综上所述,将PSMA-PET加入到先前开发的列线图中能够大幅提高其预测性能,表明PSMA-PET可能是未来预测列线图的必要候选因子之一。
原始出处:
Dennie Meijer, Pim J van Leeuwen, Matthew J Roberts et al. External Validation and Addition of Prostate-specific Membrane Antigen Positron Emission Tomography to the Most Frequently Used Nomograms for the Prediction of Pelvic Lymph-node Metastases: an International Multicenter Study. Eur Urol. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多中心研究#
121
#多中心#
86
#淋巴结#
119
#淋巴结转移#
88