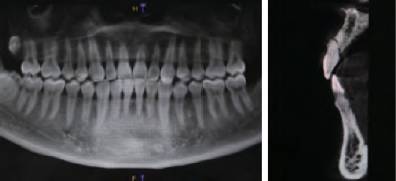
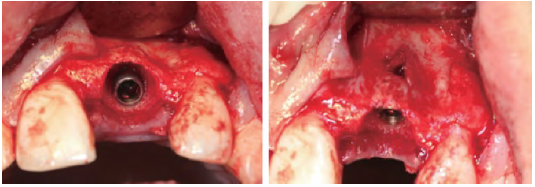
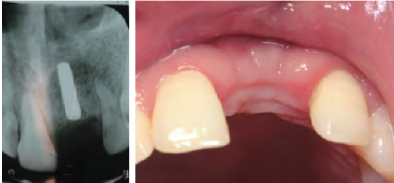
PRF联合GBR在前牙即刻种植中的应用1例
2018-11-17 孙晓琳 翟婧捷 孙悦 口腔医学研究
即刻种植方案能缩短疗程,减少拔牙后牙槽骨生理性吸收造成的种植区骨量不足,利于将种植体植入理想长轴位置,减少种植窝预备中对局部骨的损伤,保持软组织的自然形态,已逐渐受到关注。但即刻种植常伴随骨缺损,限制手术适应症,增加手术失败风险。为探讨PRF促进组织修复再生的临床效果,现将已完成修复的PRF联合GBR在前牙即刻种植中应用的病例进行报告与讨论。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#即刻种植#
82
#前牙#
77
#种植#
56
#PRF#
76
#GBR#
65