Radiology:MRI,让增殖型HCC“一眼到底”!
2021-08-21 shaosai MedSci原创
众所周知,肝细胞肝癌(HCC)在基因组、分子和组织学层面的异质性较强。越来越多的证据表明,分子和组织形态学特征之间的相关性,导致了HCC的几种组织学变体的提出。
 众所周知,肝细胞肝癌(HCC)在基因组、分子和组织学层面的异质性较强。越来越多的证据表明,分子和组织形态学特征之间的相关性,导致了HCC的几种组织学变体的提出。世界卫生组织(WHO)第五版消化系统肿瘤分类对HCC进行了重新分类,其中35%的HCC可分为组织学变体,这些HCC的组织学亚型与不同的临床和影像学特征及预后有关。
众所周知,肝细胞肝癌(HCC)在基因组、分子和组织学层面的异质性较强。越来越多的证据表明,分子和组织形态学特征之间的相关性,导致了HCC的几种组织学变体的提出。世界卫生组织(WHO)第五版消化系统肿瘤分类对HCC进行了重新分类,其中35%的HCC可分为组织学变体,这些HCC的组织学亚型与不同的临床和影像学特征及预后有关。
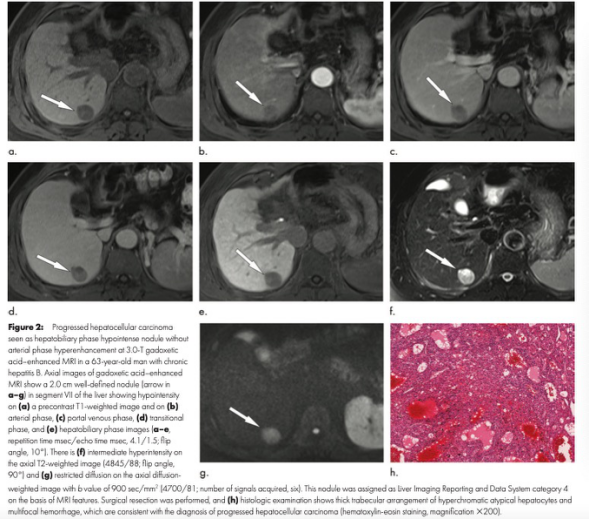
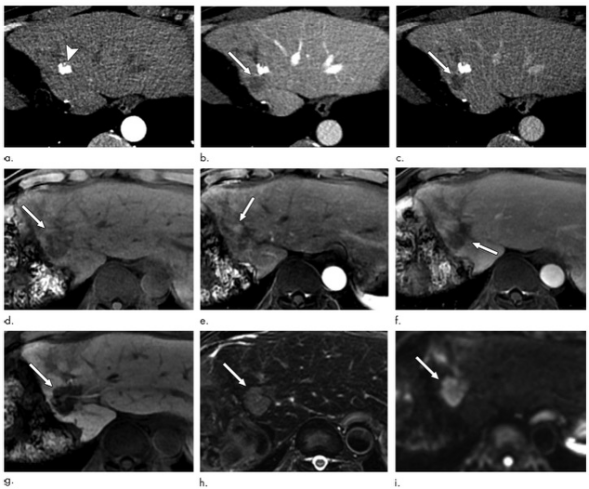
HCC的独特之处在于,在高危患者中,仅凭典型的动态影像学特征就可以进行诊断。在治疗前,在影像学上对增殖型HCC进行准确的识别有很大的治疗和预后意义。已有研究表明,不同HCC的亚型及预后与钆塞酸二钠增强MRI的成像特征之间具有相关性。肝胆特异期上的低密度HCC与高密度HCC相比,预后更差。肝胆特异期上的瘤周低密度可以预测微血管侵袭。另外,动脉期边缘高强化(APHE)和大量坏死更经常见于MTM HCC(17,18)。
为了进一步了解HCC的影像学特征与分子和组织形态学类型之间的相关性,Radiology杂志的一项研究评估了增殖型HCC的钆塞酸二钠增强MRI表现及其与术后预后的相关性,为患者术前更准确的诊断及更好的预后提供了参考依据。
本项回顾性队列研究评估了2010年1月至2013年2月期间接受肝脏切除术和术前钆塞酸二钠增强MRI检查的手术切除治疗无效的孤立HCC(≤5厘米)患者。采用Cox比例危害模型来确定总生存期(OS)、肝内远期复发和肝外转移(EM)的预测因素。平均随访时间为75.5个月±30.2(标准差)。进行多变量逻辑回归以确定与增殖型HCC相关的因素。
本共评估了158名患者(平均年龄,57岁±11;128名男性和30名女性)。158例HCC中由42例(26.6%)为增殖型HCC(17例巨块型HCC,14例角蛋白19阳性HCC,10例瘢痕型HCC,1例肉瘤型HCC)。增殖型与较差的OS(危险比[HR],3.1;95%CI:1.5,6.0;P = .01)、较高的肝内远处复发率(HR,1.83;95%CI:1.1,2.9;P = .01)和EM(HR,9.97;95%CI:3.2,31.4;P < .001)相关。钆塞酸二钠增强MRI的动脉期边缘高强化(APHE)(OR],6.35;95% CI:1.9,21.7;P = .01)和高血清甲胎蛋白(>100 ng/ml)(OR,4.18;95% CI:1.64,10.7;P = .01)是增殖型HCC的独立预测因素。边缘APHE的存在与不良的OS(HR,2.4;95% CI:1.2,4.9;P = .02)和较高的EM率(HR,7.4;95% CI:2.5,21.7;P < .01)有关。

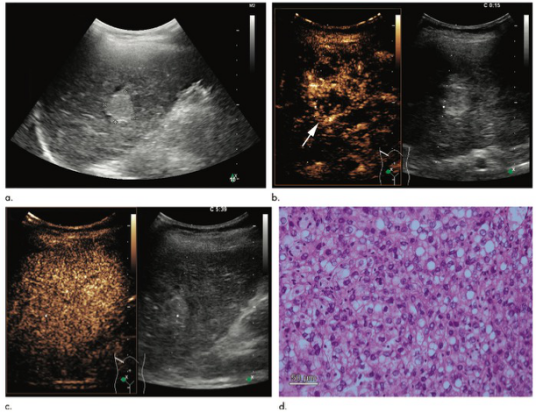
图1 78岁女性,增殖型性肝细胞肝癌(HCC)。(A)强化前图像显示一直径为3.9厘米大小的低信号强度病变,(B)钆塞酸二钠增强MRI显示的动脉期边缘高强化。(C) 大体检查时,肿瘤为一个轮廓清晰的多叶坚硬的白色肿块,有多个出血灶。(D)组织病理学特征与HCC一致,但在免疫组化中观察到角蛋白19(K19)的表达。总生存期为30个月。肝内远处复发和肝外转移分别发生在手术切除后6个月和13个月。
本研究表明,肝细胞肝癌(HCC)的增殖型分类是总生存期(OS)不佳的独立因素,同时预示着肝内远处复发和肝外转移(EM)风险的增加。术前钆塞酸二钠增强MRI的动脉期边缘高强化有助于增殖型HCC的识别,同时可预测OS不佳和EM发生率的增加。
原文出处:
Hyo-Jin Kang,Haeryoung Kim,Dong Ho Lee,et al.Gadoxetate-enhanced MRI Features of Proliferative Hepatocellular Carcinoma Are Prognostic after Surgery.DOI:10.1148/radiol.2021204352
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









感谢分享
78
影像组学发力
71
#HCC#
77
感谢分享
120