Nature重磅:艾滋病治疗最新进展!新疗法有望长期控制病毒水平
2022-08-22 生物探索 生物探索
为了减轻感染者的患病负担,一众科学家一直在探索可有效控制感染者体内病毒水平的疗法。如何研发出长期有效的艾滋病药物,成为诸多科学家的目标。
如今,抗逆转录病毒疗法可以将艾滋病感染者体内的病毒水平控制在安全范围以内,但是要终身服药,不仅会产生一定副作用,也存在诱导病毒耐药性的风险。鉴于以上问题,科学家们一直在探索可以长效控制感染者体内病毒水平的有效方法。
近期,来自美国国家过敏和传染病研究所的研究团队在艾滋病治疗方面取得了一项意义重大的突破,研究人员通过两种广谱中和单克隆抗体的联合使用,在一项1期临床试验中实现了长期有效抑制HIV的效果。相关研究成果以“Combination anti-HIV antibodies provide sustained virological suppression”为题,发表在Nature上。如果这项研究结果可以应用至临床,有望为目前的抗转录病毒疗法提供替代性治疗方案。

图1 研究成果(图源:[1])
既往研究表明,除了中和HIV的能力外,某些单克隆抗体(bNAbs)还可能介导持久性病毒的清除和增强宿主对病毒的免疫力。因此,在这项研究中,研究人员联合使用了两种与HIV包膜糖蛋白的不同区域结合的bNAbs,即3BNC117 和 10-1074。此前多项研究已经验证了这两种抗体广泛中和HIV的效果:3BNC117靶向的是HIV入侵人体的主要结合位点CD4,可以对超过80%的HIV毒株发挥作用;10-1074靶向V3聚糖位点,之前的研究也证实了其高效的广谱抗病毒活性。
在2018年9月至2021年1月期间,研究人员进行了一项Ⅰ期临床试验,以评估bNAbs 3BNC117 和 10-1074 组合在 HIV 感染者中的安全性、耐受性和有效性。这项试验包括两个组成部分,第一部分是一项随机、双盲、安慰剂对照研究。14位HIV感染者被分为实验组和对照组。其中实验组受试者在24周内接受8次3BNC117和10-1074的联合输液治疗,随后在接受第一次bNAb输注后停止了抗逆转录病毒疗法。结果显示,与对照组相比,联合疗法在实验组中的5名受试者体内完全抑制了HIV的病毒血症,抑制效果最长达到了43周,并且没有产生抗药性。而对照组的所有受试者都经历了停止治疗后体内病毒水平的反弹。此外,实验组的受试者均未出现严重不良反应。
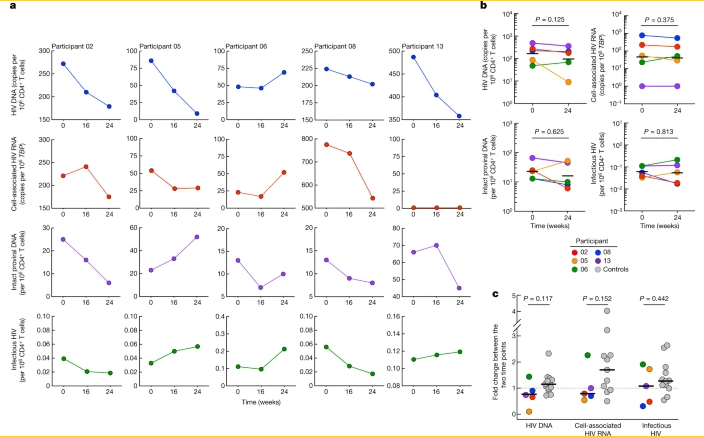
图2 停止治疗后,试验组的5名受试者体内实现了持续的病毒学抑制(图源:[1])
试验的第二部分是一项单臂、开放标签的临床试验,5名尚未接受抗逆转录病毒疗法治疗但体内HIV水平较低的感染者在24周内接受8次3BNC117和10-1074的联合输液治疗后,其中有2人实现了病毒血症的完全抑制,抑制时间平均为41.7周。
总之,这些试验结果表明,在没有进行抗逆转录病毒治疗的情况下,3BNC117和10-1074的联合疗法在长期抑制HIV病毒水平方面非常有效,前提是基线时不存在抗体性病毒。这项突破性以探究也为开发具有长半衰期的下一代抗体提供了重要指导。
但是也应该注意到,该项研究的相关数据强烈表明,在进行联合抗体治疗24周后再清除抗体,病毒水平还会反弹。因此,未来的试验需要在最后一次输注bNAb后启动预先指定的抗逆转录病毒治疗,以防止感染者出现抗体抗性病毒。
参考资料:
[1]Sneller MC, Blazkova J, Justement JS, et al. Combination anti-HIV antibodies provide sustained virological suppression. Nature. 2022 Jun;606(7913):375-381. doi: 10.1038/s41586-022-04797-9. Epub 2022 Jun 1. PMID: 35650437.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
103
#最新进展#
107
#最新#
115
#重磅#
127
#新疗法#
143