Neurology :淀粉样血管病患者,记忆变差或可反映tau病变
2021-04-29 Freeman MedSci原创
淀粉样血管病患者,记忆变差或可反映tau病变

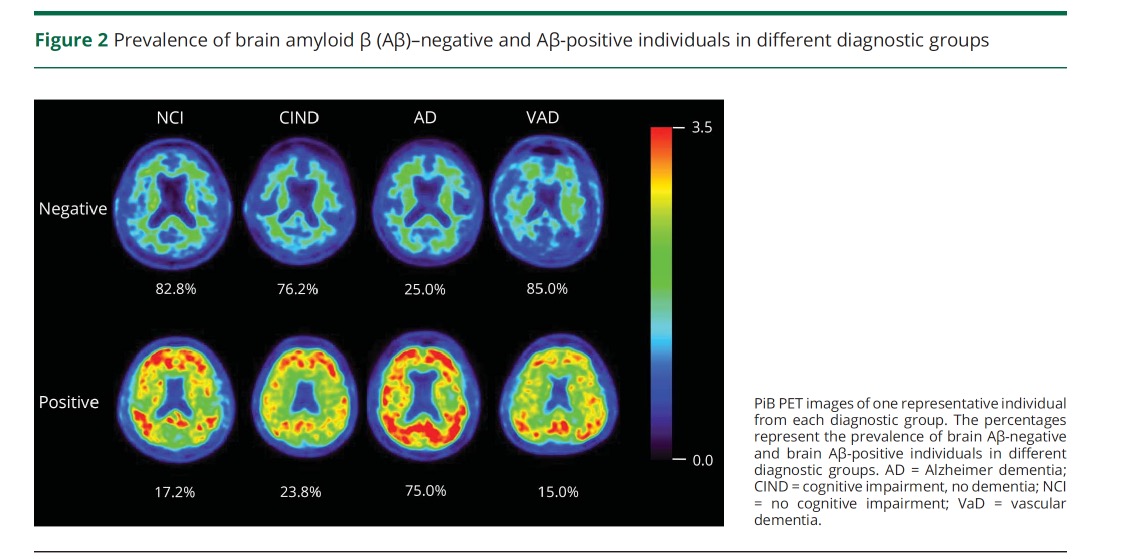
大脑淀粉样血管病(CAA)是一种以淀粉样物质在脑膜和皮质血管中的微血管沉积为特征的疾病,是导致血管性认知障碍和痴呆的一个关键因素。虽然CAA是阿尔茨海默病(AD)的一个常见伴随特征,但它是一种独立的神经病理状况,超过一半的CAA病例没有伴随AD相关的tau病理学。在临床上,区分伴有或不伴有tau病理学的CAA患者,对治疗方法和预后有重要意义。
以前对阿尔茨海默病患者的研究表明,记忆表现与内侧颞叶由tau介导的神经病理改变的严重程度密切相关,并可预测即将出现的认知衰退。鉴于这一证据,CAA患者客观记忆障碍的存在可以提供潜在的神经病理过程的相关信息,并提示伴随的tau病理学的严重程度增加。
藉此,哈佛大学医学院Dorothee Schoemaker利用tau-PET成像,探讨了记忆障碍是否与脑淀粉样血管病变(CAA)患者同时存在的tau病变有关。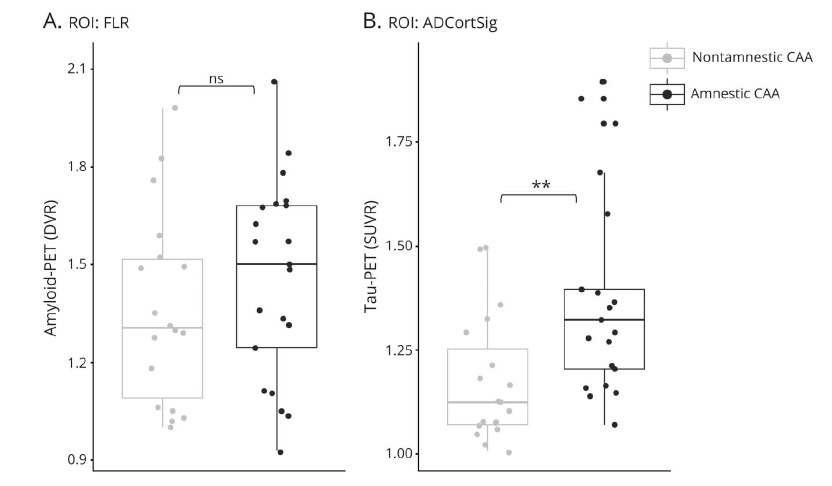
他们纳入了46名可能患有CAA的患者接受了神经心理学检查和MRI检查,以量化脑小血管疾病的结构标志物。这些参与者中的一部分还完成了[11C]-匹兹堡化合物B(n = 39)和[18F]-flortaucipir(n = 40)PET,分别用于估计淀粉样蛋白和tau负担。
根据神经心理学表现,参与者被分为失忆症和非失忆症。进行统计分析以检查认知能力、脑小血管疾病的结构性标志物以及淀粉样蛋白和tau-PET的保留在有失忆症和无失忆症的CAA参与者之间的差异。
他们发现,患有可能的CAA并有失忆表现的患者与非失忆患者相比,表现出全面的更严重的认知障碍、更小的海马体积(p < 0.001),以及在易受阿尔茨海默病神经变性影响的区域增加tau-PET结合(p = 0.003)。
患有CAA的失忆者和非失忆者在任何其他MRI标志物或淀粉样蛋白-PET结合方面没有差异。在所有评估的神经影像标志物的广义线性模型中,tau-PET(β = -0.85,p = 0.001)和海马体积(β = 0.64 p = 0.01)是预测记忆表现的唯一重要因素。CAA患者的认知特征中,Tau-PET升高的患者在记忆领域的表现明显较低(P = 0.004)。
这个研究的重要意义在于发现了,在可能的(probable)CAA患者中存在客观的记忆障碍,其可以作为潜在的tau病变的标志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管病#
0
#Neurol#
52
#Tau#
73
好文章,值得一读
92
好文章,值得一读。
88