美国警示氟喹诺酮抗生素的主动脉瘤破裂或夹层风险
2019-02-02 MedSci MedSci原创
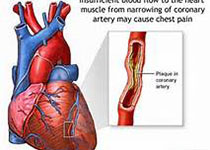
2018年12月20日,美国食品药品监督管理局(FDA)评估发现氟喹诺酮抗生素能增加罕见且严重的主动脉瘤破裂或夹层风险的发生。主动脉瘤破裂或主动脉撕裂(也称主动脉壁夹层),可导致出血危险甚至死亡,全身使用(口服、注射)氟喹诺酮抗生素可发生此风险。氟喹诺酮抗生素批准用于治疗某些细菌感染,并已上市使用了30余年。氟喹诺酮抗生素通过杀菌或抑制致病菌生长发挥疗效,如果不进行治疗,一些感染可能扩散并导致严重
2018年12月20日,美国食品药品监督管理局(FDA)评估发现氟喹诺酮抗生素能增加罕见且严重的主动脉瘤破裂或夹层风险的发生。主动脉瘤破裂或主动脉撕裂(也称主动脉壁夹层),可导致出血危险甚至死亡,全身使用(口服、注射)氟喹诺酮抗生素可发生此风险。
氟喹诺酮抗生素批准用于治疗某些细菌感染,并已上市使用了30余年。氟喹诺酮抗生素通过杀菌或抑制致病菌生长发挥疗效,如果不进行治疗,一些感染可能扩散并导致严重健康问题。和其他抗生素一样,氟喹诺酮不用于治疗病毒感染,如感冒、流感或健康人群的支气管炎。氟喹诺酮抗生素用于治疗氟喹诺酮敏感菌的感染时,其获益大于风险,如肺炎或腹腔感染。氟喹诺酮抗生素常见不良反应包括恶心、腹泻、头痛、头晕、头昏眼花或失眠。
FDA检索了其不良事件报告系统(FAERS)数据库的病例报告并评估了4项流行病学研究,以审查使用氟喹诺酮抗生素和主动脉瘤和夹层风险的相关性。以上数据表明主动脉瘤或夹层形成的风险升高与使用氟喹诺酮相关。但评估的4项流行病学研究不能确定此风险的潜在机制,主动脉瘤的背景风险在不同人群中也有差异。多项研究均显示,与普通人群相比,使用氟喹诺酮患者主动脉瘤破裂和夹层风险约为2倍,基于以上评估及研究结果,FDA决定发布警示信息以提醒医务人员和患者:除非没有其他治疗选择,氟喹诺酮不应用于风险增加的患者,例如有动脉或其他血管阻塞病史或血管瘤(异常隆起)、高血压、某些涉及血管变化的遗传性疾病以及老年患者。FDA要求所有氟喹诺酮抗生素的产品说明书和患者用药指南中增加此风险的新的警告信息。
针对医务人员信息:
应避免给患有动脉瘤或有动脉瘤风险的患者处方氟喹诺酮抗生素,如外周动脉粥样硬化血管疾病、高血压、某些遗传疾病(如马凡综合征和埃勒斯-丹洛斯综合征)以及老年患者;只有在没有其他治疗选择时,才能给这些患者处方氟喹诺酮抗生素。劝告患者改变生活方式,这样可以帮助降低主动脉瘤进展的风险,包括戒烟、健康饮食、控制相关疾病如高血压和高胆固醇症。对动脉瘤患者进行主动脉瘤的常规检查和治疗可以帮助预防瘤的生长和破裂。劝告诊断有动脉瘤患者如果发生了主动脉瘤生长的任何体征或症状立即就医,症状包括:胃部区域有跳动感,后背或胃部区域的深部疼痛,持续数小时或数天的胃部区域持续绞痛,下巴、颈部、背部或胸部疼痛,咳嗽或声音嘶哑,呼吸急促、呼吸或吞咽困难等。
针对患者信息:
如果出现了胃部、胸部或背部突发的严重且持续疼痛应立即就医。应意识到主动脉瘤一般不会有症状直到瘤变大或破裂,因此如果使用氟喹诺酮抗生素出现任何不常见的副作用应立即报告医务人员。在开始抗生素治疗之前,如果有动脉瘤、阻塞或硬化、高血压、或某些遗传疾病如马凡综合征或埃勒斯-丹洛斯综合征应告知医生。如果已经在使用氟喹诺酮抗生素抗感染,在咨询医生前不要擅自停药。
参考文献
1. Lee CC, Lee MG, Chen YS, et al. Risk of Aortic dissection and aortic aneurysm in patients taking oral fluoroquinolone. JAMA Int Med 2015;175(11):1839-1847.
2. Pasternak B, Inghammar M, Svanstrom H. Fluoroquinolone use and risk of aortic aneurysm and dissection: nationwide cohort study. BMJ. 2018;360:k678.
3. Daneman N, Lu H, Redelmeier DA. Fluoroquinolones and collagen associated severe adverse events: a longitudinal cohort study. BMJ Open. 2015;5(11):e010077.
4. Lee CC, Lee MG, Hsieh R, et al. Oral fluoroquinolone and the risk of aortic dissection. J Am Coll Cardiol. 2018;72(12):1369-1378.
5. Howard DPJ, Banerjee A, Fairchild JF, et al. Age-specific incidence, risk factors and outcome of acute abdominal aortic aneurysms in a defined population. BJS 2015;102:907- 915.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#喹诺酮#
0
谢谢,谢谢分享
97
学习,谢谢分享
103
#主动脉#
49
#主动脉瘤#
50
#氟喹诺酮#
69
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
93
学习谢谢分享
91