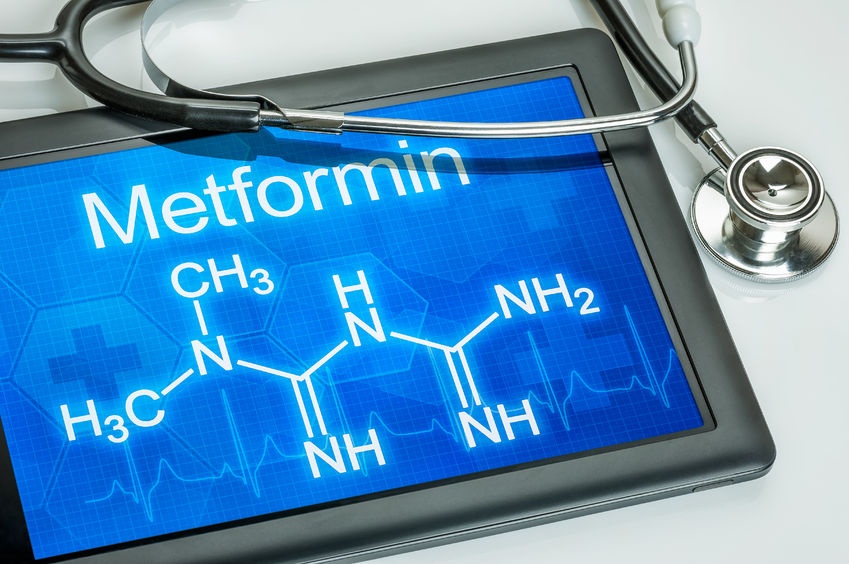
Nat Med:科学家揭秘“神药”二甲双胍降糖之谜!
2017-05-27 Chen 生物探索
5月22日,发表在Nature Medicine杂志上题为“Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug”的研究中,来自瑞典、西班牙等国的一个国际研究小组发现,二甲
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
47
新的发现,学习了。
101
#Med#
48
努力学习!有用的
102
学习了谢谢分享
104
学习了
99