Diabetes Care:多篇新发糖尿病患者长期随访研究提示,早期控糖真的很重要!
2021-10-12 MedSci原创 MedSci原创
不论年轻人还是老年人,良好的血糖控制必须尽早开始,并持续保持。
糖尿病控制与并发症试验(DCCT)和英国前瞻性糖尿病研究(UKPDS)使我们对糖尿病的自然史和管理有了基本的了解。其中包括强有力的证据:1)加强血糖管理可以限制糖尿病的一些并发症;2)HbA1c水平与并发症风险之间存在剂量反应关系;3)HbA1c<7.0%(<53mmol/mol)的治疗目标是现实的和适当的。
在研究计划结束后,对随机队列的持续观察进一步表明,在随机治疗阶段无法显示出心血管事件和死亡率的改善,但在两组的血糖控制持平后的很长一段时间内,心血管事件和死亡率明显降低。在这两项研究中,由HbA1c评估的血糖控制在统计学上占了结果差异的大部分。
在近期《糖尿病护理》Diabetes Care的三篇文章中,DCCT和UKPDS研究者提供了更多关于在糖尿病自然史早期加强血糖控制的长期效果的信息。在两篇文章中的第一篇是基于对糖尿病干预和并发症流行病学(EDIC)研究中DCCT队列20多年的额外观察,报告了对微血管并发症数据的新分析。
这些数据补充了之前报道的证据,即尽管在停止随机比较治疗后不久两组的HbA1c值趋于一致,但在最初强化管理的队列中,微血管疾病的进展率持续较低。研究者们以前曾将这种现象称为 "代谢记忆"。在此,他们进一步报告了10年后结果差异的逐渐减弱。他们强调了对微血管并发症的增量效应和整个观察期的累积效应之间的区别,后者导致随机分组之间的持久差异。
在第二篇文章中,Lachin等人报告了在EDIC的20年观察期间,较早与较晚改善血糖控制对结果的影响的模型估计。他们比较了不同时间段的10年HbA1c 7.0.% (53 mmol/mol)与HbA1c 9.0% (75 mmol/mol)的效果。
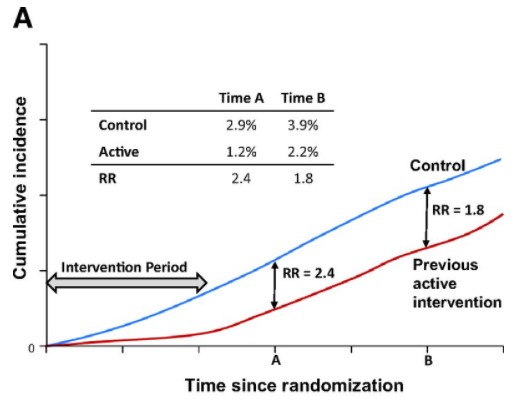
在随机干预期间和停止干预后,高血糖的影响的替代模式。
这些模型估计,在20年的观察期间,与HbA1c 9.0%相比,7.0%的患者的心血管事件危险的减少超过50%;而HbA1c 开始为9.0%后将至7.0%减少仅为12%。同样,他们估计,较早地控制HbA1c 10年将使估计肾小球滤过率<60 mL/min/1.73 m2的新发病率减少>60%,而较晚地减少将导致危险性仅减少20%。
综上,不论年轻人还是老年人,良好的血糖控制必须尽早开始,并持续保持。
参考文献:
Lingering Effects of Hyperglycemia in Recently Diagnosed Diabetes During Long-term Follow-up of the DCCT/EDIC and UKPDS Cohorts: More Evidence That Early Control Matters. Diabetes Care 2021 Oct; 44(10): 2212-2215. https://doi.org/10.2337/dci21-0030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#BET#
57
#DIA#
59
#Diabetes#
78
#长期随访#
81
#随访研究#
133
#糖尿病患者#
51
学习了#学习#
165
good
100
赞
92