J Clin Endocrinol Metab:Elagolix会以剂量依赖性的方式抑制女性排卵
2021-01-19 MedSci原创 MedSci原创
Elagolix是一种口服促性腺激素释放激素(GnRH)拮抗剂,最近被批准用于治疗子宫内膜异位症相关疼痛,并正在开发用于子宫肌瘤相关的大量月经出血。近期,一项随机、开放标签、多中心研究评估了Elago
Elagolix是一种口服促性腺激素释放激素(GnRH)拮抗剂,最近被批准用于治疗子宫内膜异位症相关疼痛,并正在开发用于子宫肌瘤相关的大量月经出血。近期,一项随机、开放标签、多中心研究评估了Elagolix对排卵和卵巢性激素的影响,结果显示Elagolix对女性卵巢储备的影响不大。
研究纳入18至40岁的健康排卵期女性,口服给药Elagolix,连续3次,每次28天,每次100至200mg,每天一次(QD),100至300mg,每天两次(BID),300mg BID加醋酸雌二醇/去甲孕酮(E2/NETA)1/0.5mg QD。主要结果测量是经阴道超声测量的排卵率,孕酮浓度和激素抑制。
结果显示,Elagolix抑制了排卵,以剂量依赖的方式抑制排卵。100mg QD时排卵的妇女比例最高(78%),150和200mg QD和100mg BID时居中(47%-57%),200和300mg BID时最低(分别为32%和27%)。在Elagolix 300 mg BID中加入E2/NETA可进一步抑制排卵率至10%。Elagolix还以剂量依赖性方式抑制黄体生成素和卵泡刺激素,导致雌二醇和孕酮受到剂量依赖性抑制。与筛查周期相比,Elagolix对卵巢储备的血清生物标志物没有影响,降低了子宫内膜厚度。
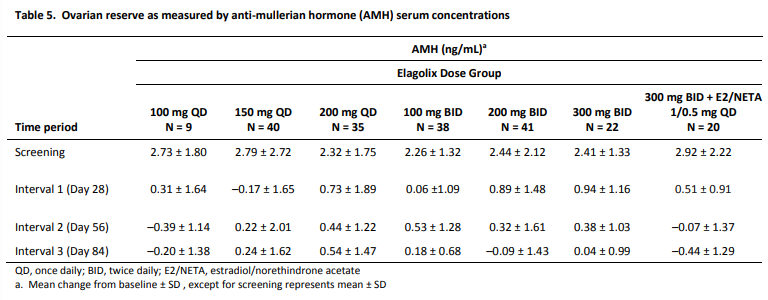
综上所述,该研究结果表明,Elagolix对卵巢储备的影响不大。接受Elagolix治疗的女性也可能会排卵,应采取有效的避孕方法。使用elagolix 300 mg BID加E2/NETA 1/0.5 mg QD的方案,女性排卵率最低。
原始出处:
David F Archer, Juki Ng, et al., Elagolix Suppresses Ovulation in a Dose-Dependent Manner: Results From a 3-Month, Randomized Study in Ovulatory Women. J Clin Endocrinol Metab. 2020 Mar 1;105(3):dgz086. doi: 10.1210/clinem/dgz086.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Meta#
53
#排卵#
67
#MET#
58
#Elagolix#
63
学习
113
好
103