NEJM:HSV-1G207溶瘤病毒疗法治疗儿童高级别胶质瘤
2021-04-15 MedSci原创 MedSci原创
瘤内注射G207或联合放疗可显著缓解复发或进展型儿童高级别胶质瘤患者病情,且耐受性良好
高级别胶质瘤占儿童脑瘤的8%-10%,其恶性程度高,病情发展迅速,近日30年来,患者存活率无显著改善。目前临床上,接受标准放疗和化疗治疗的新发恶性高级胶质瘤患者的3年无事件生存率仅为11%-22%,复发患者的平均预期寿命仅5.6个月。儿童高级别胶质瘤在免疫上基本无响应,很少有肿瘤浸润淋巴细胞。溶瘤病毒治疗是一种很有前途的治疗癌症的新方法。它利用基因工程或天然病毒,在不伤害正常细胞的情况下选择性地复制并杀死癌细胞。临床前研究中,儿童脑肿瘤对基因工程单纯疱疹病毒1型(HSV-1)G207溶瘤病毒疗法高度敏感。
近日研究人员开展I期临床研究,评估了G207溶瘤病毒疗法的疗效及安全性。

本次研究采用3+3设计,经活检证实复发或进展型幕上脑肿瘤患儿参与。研究人员首先在患者脑部放置肿瘤内导管,随后第二天,患者接受了G207输注。第3组和第4组患者在G207给药后24小时内接受放疗(5Gy)。通过培养和聚合酶链反应分析对唾液、结膜和血液中的病毒脱落进行评估。通过免疫组织化学分析,检测治疗前后组织样本中肿瘤浸润的淋巴细胞。
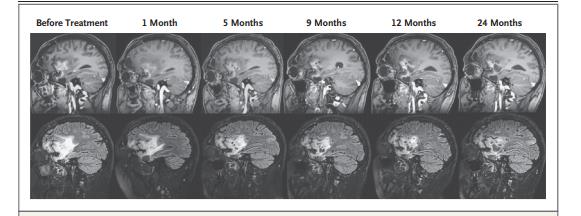
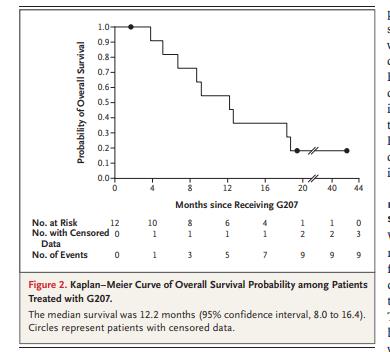
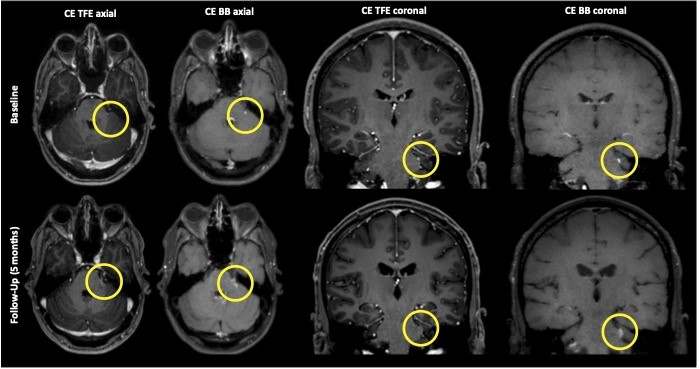
12例高级别胶质瘤患者接受G207治疗,年龄范围7-18岁。未发现与G207治疗相关的剂量限制性毒性反应或严重不良事件。报告了20例1级不良事件,可能与G207治疗有关。未发现病毒脱落。11例患者出现影像学、神经病理学或临床缓解,患者平均总生存期为12.2个月。截至2020年6月5日,11名治疗应答患者中有4名,在治疗后18个月仍存活。G207能显著增加肿瘤浸润淋巴细胞的数量。
研究发现,瘤内注射G207或联合放疗可显著缓解复发或进展型儿童高级别胶质瘤患者病情,且耐受性良好。
原始出处:
Gregory K. Friedman et al. Oncolytic HSV-1 G207 Immunovirotherapy for Pediatric High-Grade Gliomas. N Engl J Med, April 10, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HSV-1#
78
#HSV#
77
胶质瘤
81
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
78