Lancet:埃索美拉唑和阿司匹林预防Barrett食管疗效如何?
2018-07-27 xing.T MedSci原创
由此可见,高剂量PPI和阿司匹林预防治疗,特别是联合治疗,可以显著并安全地改善Barrett食管患者的预后。
食管腺癌是全球癌症死亡的第六大常见原因,Barrett食管是其最大的危险因素。近日,顶级杂志Lancet上发表了一篇研究文章,研究人员的目的是评估高剂量质子泵抑制剂(PPI)埃索美拉唑和阿司匹林对改善Barrett食管患者预后的疗效。
阿司匹林和埃索美拉唑预防Barrett化生试验是一项2×2因子设计,并在英国84个中心和加拿大的1个中心完成。Barrett食管1 cm或以上的患者按1:1:1:1的比例随机分组,分别接受高剂量(40mg每日两次)或低剂量(20mg每日一次)PPI,有或没有阿司匹林(英国每天300mg,加拿大每天325mg)治疗至少8年。报告病理学家对治疗分组不知情。该研究的主要复合终点是发生全因死亡、食管腺癌或高度不典型增生的时间,其中加速失败时间模型分析调整了所有患者的最小化因素(年龄、Barrett食管长度、肠上皮化生)。
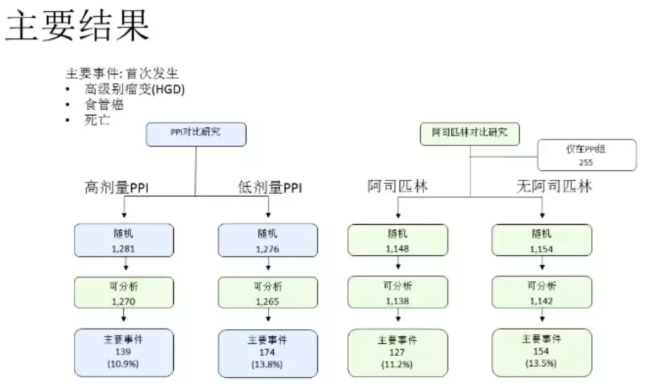
在2005年3月10日至2009年3月1日期间,该研究共招募了2557名患者。705例患者接受低剂量PPI和无阿司匹林治疗,704例患者接受高剂量PPI和无阿司匹林治疗,571例患者接受低剂量PPI和阿司匹林治疗,577例患者接受高剂量PPI和阿司匹林治疗。中位随访和治疗持续时间为8.9年(IQR为8.2-9.8),研究人员收集了20095例随访者每年和99.9%的计划数据。该研究共发生了313起主要事件。高剂量PPI(1270例患者中有139例)优于低剂量PPI(1265例患者中有174例;时间比[TR]为1.27,95%CI为1.01-1.58,P=0.038)。阿司匹林组(1138例患者中有127例事件)并未显著优于无阿司匹林组(1142例患者中有154例事件; TR为1.24,0.98-1.57,P=0.068)。如果使用非甾体类抗炎药的患者在首次使用时进行检查,阿司匹林组明显优于无阿司匹林组(TR为1.29,1.01-1.66,P=0.043; n=2236)。与不服用阿司匹林的低剂量PPI组相比,高剂量PPI与阿司匹林相结合的效果最强(TR为 1.59,1.14-2.23,P=0.0068)。需要治疗的人数对于PPI为34人,阿司匹林为43人。只有28名(1%)参与者报告了与研究治疗相关的严重不良事件。
由此可见,高剂量PPI和阿司匹林预防治疗,特别是联合治疗,可以显著并安全地改善Barrett食管患者的预后。
原始出处:
Janusz A Z Jankowski,et al. Esomeprazole and aspirin in Barrett's oesophagus (AspECT): a randomised factorial trial. Lancet 2018. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31388-6/fulltext
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
58
#RET#
66
#Barrett食管#
81
#食管#
57
#埃索美拉唑#
67
#Barrett#
80
谢谢梅斯提供这么好的信息,学到很多
89