病例分享:初诊且病情较重的T2DM患者,降糖方案如何选?
2018-11-14 韩文霞 卡路里 中国医学论坛报
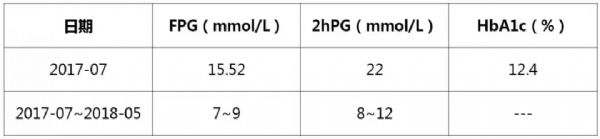
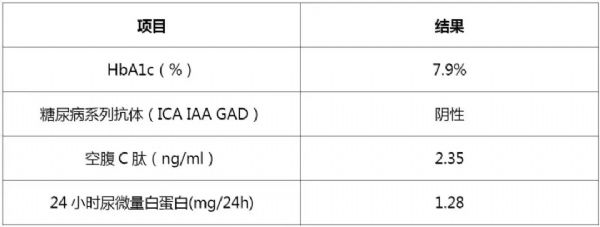
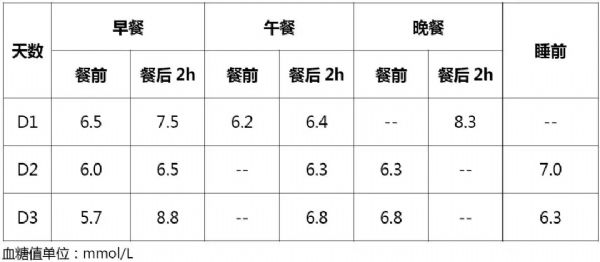
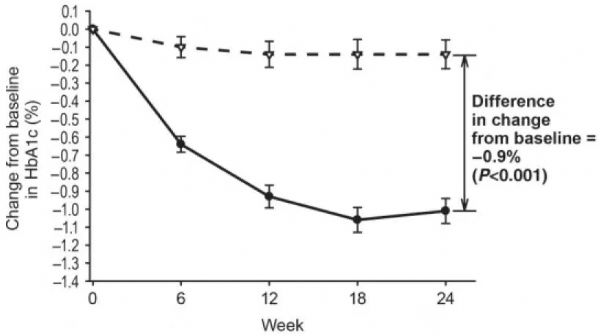
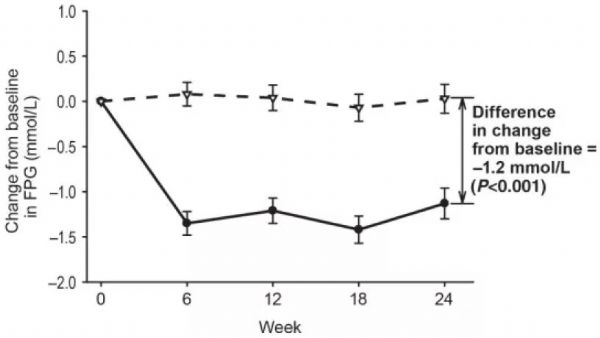
很多糖尿病防治意识不足的患者,在初诊2型糖尿病时已处于较为严重的疾病阶段,甚至出现相关并发症。对于该类患者,临床可能需要给予胰岛素强化治疗,同时辅以口服降糖药物。口服降糖药种类繁多,如何在综合考虑降糖疗效与安全性、耐受性的同时,为患者制定个体化的降糖方案,是内分泌科临床医生都需要掌握的技能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#T2DM患者#
68
#病情#
64
1
103
1
118
1
107
1
81
1239
86
学习了
60
很好
0