European Radiology:定量动态增强MRI对乳腺纤维上皮肿瘤不同组织学分级的评估
2021-11-22 shaosai MedSci原创
乳腺纤维上皮肿瘤(PT)是一种罕见的纤维上皮肿瘤,约占所有乳腺肿瘤的0.5-1%,占所有纤维上皮乳腺肿瘤的2-3%。

乳腺纤维上皮肿瘤(PT)是一种罕见的纤维上皮肿瘤,约占所有乳腺肿瘤的0.5-1%,占所有纤维上皮乳腺肿瘤的2-3%。根据2012年出版的最新版WHO乳腺肿瘤分类,乳腺PT在组织学上分为良性、边缘性和恶性,其依据是基质细胞和非典型性、有丝分裂计数、基质过度生长以及肿瘤边界的排序。乳腺PT的局部复发和远处转移的风险是不同的。良性PT的局部复发率从5%到30%不等,边缘型和恶性PT的局部复发率从30%到65%不等。PTs的组织学分级一般与预后相关。提高PTs组织学分级的术前鉴别诊断,有利于手术计划的制定,并可能在一定程度上改善预后。
乳腺钼靶、超声和MRI是无创评估乳腺肿瘤的主要成像方式。与乳腺钼靶和超声相比,多参数MRI由于具有多种定性和定量参数,有助于区分良性和恶性乳腺肿瘤并预测预后。
最近,有报道称定量动态对比增强MRI(qDCE- MRI)对乳腺肿瘤的术前诊断和病理特征有较大价值。基于模型的qDCE-MRI可以提供多个定量参数,以描述组织灌注、微血管通透性和肿瘤的血管外间隙。然而,据我们所知,还没有研究应用qDCE-MRI对乳腺PT进行组织学分级的文献报道。
近日,发表在European Radiology杂志的一项研究探讨了与肿瘤大小和ADC值相比,由qDCE-MRI得出的定量灌注参数在区分PT等级方面的预测价值,为PT的诊断提供了更准确的影像学手段。
本项回顾性研究纳入了2016年4月至2020年7月的67例乳腺PT(26例良性病变,25例边缘性病变,16例恶性病变)。使用Spearman等级相关系数将qDCE-MRI得出的灌注参数(Ktrans、kep、ve、iAUC60)、肿瘤大小以及平均ADC值与组织学等级相关联。还计算并比较了三种组织学等级的Ktrans、kep、ve、iAUC60。
肿瘤大小与组织学等级的Spearman相关系数为0.578(P<0.001);ADC值与乳腺PT的组织学等级没有相关性(P=0.059)。良性乳腺PT的Ktrans、kep、ve、iAUC60明显低于边缘型乳腺PT(p < 0.001),低于恶性乳腺PT(p < 0.001)。相比之下,边缘型乳腺PTs的Ktrans、kep、ve、iAUC60明显低于恶性乳腺PTs(分别为p < 0.001、p < 0.001、p = 0.007)。在ROC分析中,Ktrans、kep、ve、iAUC60的AUC高于使用肿瘤大小和ADC值来区分三个PT等级的AUC。
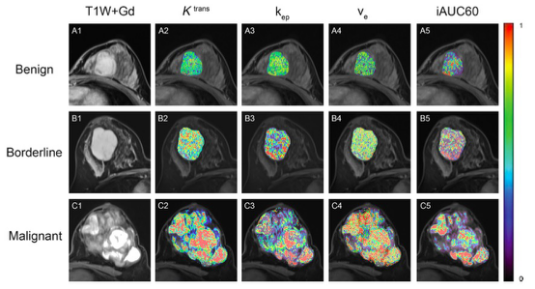
图 3名女性患者的增强后轴位T1加权MRI图像和qDCE-MRI扫描得出的Ktrans、kep、ve、iAUC60图,分别为良性(42岁,Ktrans=0.0996 min-1,kep=0.2858 min-1,ve=0.3481,iAUC60=0.1355,A1-A5),边缘型(44岁,Ktrans=0.1903 min-1,kep=0.3990 min-1,ve=0.4770,iAUC60=0.2865,B1-B5)和恶性(42岁,Ktrans=0.2763 min-1,kep=0.4443 min-1,ve=0.6232,iAUC60=0.3519,C1-C5)PTs。
本项研究表明,从qDCE-MRI得出的定量和半定量的灌注参数(Ktrans、kep、ve、iAUC60,特别是Ktrans)显示出比肿瘤大小和ADC更好的诊断效能,因此本研究提示qDCE-MRI有助于术前乳腺PT的鉴别及等级的确定。
原文出处:
Zhilong Yi,Mingwei Xie,Guangzi Shi.Assessment of quantitative dynamic contrast-enhanced MRI in distinguishing different histologic grades of breast phyllode tumor.DOI:10.1007/s00330-021-08232-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#动态增强MRI#
70
#组织学#
89
#上皮肿瘤#
93
#PE#
55