Cardiovasc Diabetol:恩格列净对稳定性慢性心力衰竭患者酮体水平的影响
2021-11-21 MedSci原创 MedSci原创
稳定型CHF患者服用恩格列嗪后酮体增加。这一增加导致恩格列嗪对血压和血管参数的有益作用减弱。
最近的研究表明,钠-葡萄糖协同转运蛋白2(SGLT-2)抑制剂可增加1型和2型糖尿病患者血液中酮体的水平。其他研究表明,在慢性心力衰竭(CHF)患者中,酮体作为燃料基质可增加心肌需氧量,特别是β-羟基丁酸酯(β-OHB)可能通过损害内皮依赖性舒张而增加血压(BP),从而导致血管硬度增加。本研究评估了SGLT 2抑制剂恩格列净是否会增加稳定型CHF患者的酮水平体,以及这种增加是否会损害血压和血管功能。

在这项前瞻性、双盲、安慰剂对照、平行组单中心研究中,75名CHF患者(左室射血分数39.0±8.2%)随机(2:1)接受恩格列嗪口服治疗(10mg/次/天 )或安慰剂治疗,72名患者完成了该研究。通过24小时动态血压(ABP)监测评估基线血压,通过血压计系统评估血管硬度参数,并通过酶分析评估空腹代谢参数,包括β-OHB。治疗12周后重复相同的测量。在72名患者中,19名患者的血清β-OHB水平低于分析的下限(<0.05 mmol/l),因此被排除在后续分析之外。
这项研究的主要发现是,与安慰剂组相比,稳定型CHF患者中,使用恩格列嗪治疗12周会导致空腹血清β-OHB升高。在对患有急性心肌梗死的T2DM患者进行的人体研究中,与安慰剂组相比,恩格列嗪组血液中的酮体倾向于增加。此外,在T1DM患者中,2.5 mg恩格列嗪和安慰剂的酮症酸中毒率相当,但在10 mg和25 mg时有所增加。已证明使用SGLT2抑制剂治疗可增加1型和2型糖尿病患者的血β-OHB水平。通过恩格列嗪治疗12周的疗效,可以观察到血压和血管功能显著改善。治疗12周后,收缩压显著下降。然而,舒张压没有任何显著改善。
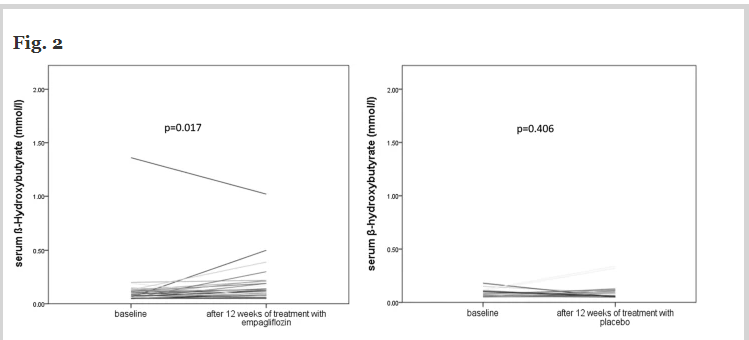
恩格列嗪治疗12周后和安慰剂疗12周后基线间β-羟基丁酸(β-OHB)的变化(左侧)
在目前的研究中,发现血管硬度和血压的改善与血清β-OHB的增加呈负相关,表明β-OHB的增加与中枢血压和24小时ABP的改善程度较低有关。中枢血压和24小时ABP都被认为是心血管事件和总体死亡率的强独立预测因子。
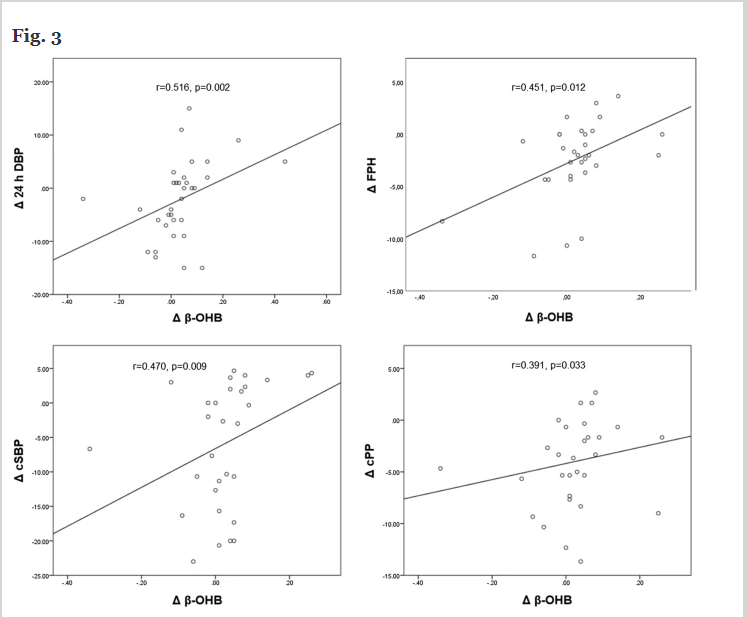
β-羟基丁酸酯、血压和血管参数变化之间的关系
有趣的是,研究结果表明,在使用恩格列嗪治疗后,β-OHB的增加产生了负面影响,稳定型CHF患者服用恩格列嗪后酮体增加。这一增加导致恩格列嗪对血压和血管参数的有益作用减弱。
参考文献:Pietschner, R., Kolwelter, J., Bosch, A. et al. Effect of empagliflozin on ketone bodies in patients with stable chronic heart failure. Cardiovasc Diabetol 20, 219 (2021). https://doi.org/10.1186/s12933-021-01410-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#稳定性#
90
#BET#
92
#ASC#
67
#DIA#
65
#慢性心力衰竭#
106