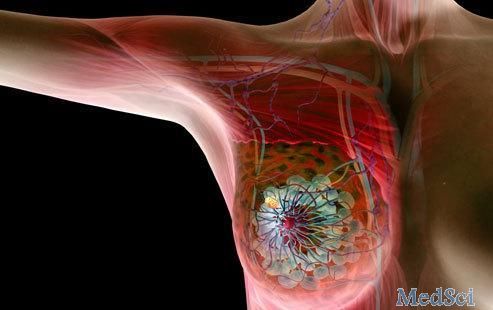
Lancet oncol:帕妥珠单抗+曲妥珠单抗+多西他赛治疗HER2+转移性乳腺癌的8年预后
2020-03-17 MedSci原创 MedSci原创
CLEOPATRA试验是一个3期的研究,对比帕妥珠单抗+曲妥珠单抗+多西他赛和安慰剂+曲妥珠单抗+多西他赛用于HER2+转移性乳腺癌的疗效和安全性。在主要分析报告中,与安慰剂组对比,帕妥珠单抗组的无进
CLEOPATRA试验是一项在全球25个国家的204个中心开展的双盲的、安慰剂为对照的3期临床试验,招募年满18岁的HER2阳性的既往未进行过化疗或生物学治疗的转移性乳腺癌患者。所有药物通过静脉给予,3周一疗程。主要结点是经独立评估的无进展生存期。
2008年2月12日-2010年7月7日,共评估了1096位患者,其中808位被招募及随机分组。402位被分至实验组(帕妥珠单抗+曲妥珠单抗+多西他赛),406位被分子安慰剂组(安慰剂+曲妥珠单抗+多西他赛)。本次分析的时间结点为2018年11月23日。从2012年7月-2018年11月,有50位患者从安慰剂组转至实验组。实验组和安慰剂组的中位随访时间分别是99.9个月个98.7个月;两组8年
的存活率分别为37%和23%。最常见的3-4级副作用是中性粒细胞减少(实验组:200例[49%] vs 安慰剂组183例[46%])。实验组408位患者中有5位(1%)、安慰剂组396位患者中有6例(2%)治疗相关死亡。
本次分析表明既往观察到的帕妥珠单抗、曲妥珠单抗和多西他赛与安慰剂、曲妥珠单抗和多西他赛的总体生存率的改善在中位随访8年以上的患者后得以维持。帕妥珠单抗、曲妥珠单抗和多西他赛联合疗法的长期安全性和心脏安全性在总人群和交叉患者中得以维持。HER2靶向治疗改变了HER2阳性转移性乳腺癌的自然史帕妥珠单抗和曲妥珠单抗+多西他赛的双重阻断治疗的8年总生存率达到37%。
原始出处:
Sandra M Swain, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. The Lancet Oncology. 12 March, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曲妥珠#
0
#Lancet#
60
#Oncol#
62
#转移性#
64
谢谢梅斯分享这么多精彩信息
90