Neurology:脑淀粉样血管病和高血压性小血管病腔隙分布有何差异?
2017-05-06 xing.T MedSci原创
由此可见,脑叶腔隙与CAA相关,而深部的腔隙在HTN-SVD患者中更频繁。脑叶腔隙似乎与WMH关系密切,提示它们可能有共同的起源。
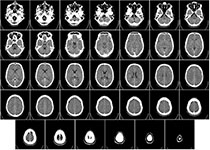
近日,神经病学领域权威取杂志Neurology上发表了一篇研究文章,研究人员旨在探讨根据波士顿标准确诊的/极大可能的脑淀粉样血管病(CAA)脑出血(ICH)患者和高血压小血管疾病(HTN-SVD;基底节、丘脑、脑干部位的脑出血)患者之间深部和脑叶腔隙是否有差异。
研究人员确定了深部和脑叶的腔隙,类似于用于脑出血和脑微出血(CMBs)的区域分布。然后研究人员比较CAA-ICH患者以及严格深部CMB和ICH(HTN-ICH)患者之间腔隙的分布。研究人员采用多变量模型的评估了腔隙位置与CAA-ICH和HTN-ICH诊断之间的独立相关性。在调整年龄和经过验证的可视化量表后,研究人员采用偏相关分析评估了脑叶腔隙与白质高信号(WMH)体积之间的相关性。
在该研究中最后有316例ICH患者纳入队列,腔隙在参与者中较为常见(24.7%),在191例CAA患者和125例HTN-ICH患者中有相似的发生率(23% vs. 27.2%,P=0.4)。脑叶腔隙在CAA患者中更为常见(20.4% vs. 5.7%,P<0.001),而深部腔梗在HTN-ICH患者中更常见(15.2% vs. 2.1%,P<0.001)。将人口学和SVD的临床及神经影像学标志物进行校正后,脑叶腔隙与CAA相关(P=0.003),而深部腔隙与HTN-ICH相关(P<0.001)。调整年龄后,80%的脑叶腔隙至少与WMH有关,它们与WMH体积高度相关(r=0.42,P<0.001)。
由此可见,脑叶腔隙与CAA相关,而深部的腔隙在HTN-SVD患者中更频繁。脑叶腔隙似乎与WMH关系密切,提示它们可能有共同的起源。
原始出处:
Marco Pasi, et al. Distribution of lacunes in cerebral amyloid angiopathy and hypertensive small vessel disease. Neurology. 2017. http://dx.doi.org/10.1212/WNL.0000000000004007
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脑淀粉样#
47
#血管病#
67
#小血管病#
85
#高血压性#
66
#Neurol#
45
不错的方式,努力学习,刻苦专研,不断总结出来新经验。
81
学习了,谢谢分享
0
学习了,表现和潜在的机制
76
#脑淀粉样血管病#
68
哪来那么多的病例
120