Lancet:社区获得性肺炎住院患者3天抗生素治疗病情稳定后即可停药
2021-03-26 MedSci原创 MedSci原创
对于β-内酰胺类抗生素治疗3天后病情稳定的社区获得性肺炎住院患者,立即停药人群的预后与8天抗生素治疗人群相当
下呼吸道感染是使用抗生素的最常见适应症之一。在美国,社区获得性肺炎每年导致60万至80万人入院,其中65岁及以上人群的发病率最高。在过去十年中,由于全球人口老龄化,社区获得性肺炎和相关死亡的病例数不断增加。缩短社区获得性肺炎住院患者的抗生素治疗时间有助于减少抗生素消耗,减少细菌耐药性、不良事件和相关成本。

本研究的目的是评估在治疗3天后病情稳定的社区获得性肺炎患者是否需要额外5天的β-内酰胺抗生素治疗。
研究人员在法国的16个医疗中心进行了这项双盲、随机、安慰剂对照、非劣效性试验。成人患者(年龄≥18岁)因中重度社区获得性肺炎入院(无需ICU治疗),且在接受β-内酰胺抗生素治疗3天后符合临床病情稳定标准,随机分配接受继续β-内酰胺治疗(口服阿莫西林1 g+克拉维酸125 mg,一天三次)或安慰剂,持续5天。研究的主要结果是首次服用抗生素后15天治愈,定义为体温≤37.8℃,呼吸系统症状缓解或改善,并且没有任何原因的额外抗生素治疗。非劣性边界为10%
研究对总计706名患者进行了资格评估,在β-内酰胺治疗3天后,310人随机分配接受安慰剂(n=157)或继续β-内酰胺治疗(n=153)。在ITT人群中,中位年龄为73.0岁,41%为女性。在ITT分析中,安慰剂组152名参与者中有117名(77%)在第15天治愈,β-内酰胺组151名参与者中有102名(68%)在第15天治愈(组间差异为9.42%),达到非劣效性终点。方案分析中,安慰剂组145名参与者中的113名(78%)和β-内酰胺治疗组146名参与者中100名(68%)在第15天治愈(差异为9.44%),达到非劣效性。组间不良事件发生率相似(安慰剂组152例中有22例出现不良事件[14%],β-内酰胺组151例中有29例 [19%])。最常见的不良事件是消化系统疾病,安慰剂组152例患者中有17例(11%)出现消化系统疾病,β-内酰胺组151例患者中有28例(19%)。到第30天,安慰剂组有3名(2%)患者死亡(1名死于金黄色葡萄球菌引起的菌血症,1名死于急性肺水肿后的心源性休克,1名死于与急性肾功能衰竭相关的心力衰竭),β-内酰胺组有2名(1%)患者死亡(死于肺炎复发和可能的急性肺水肿)。
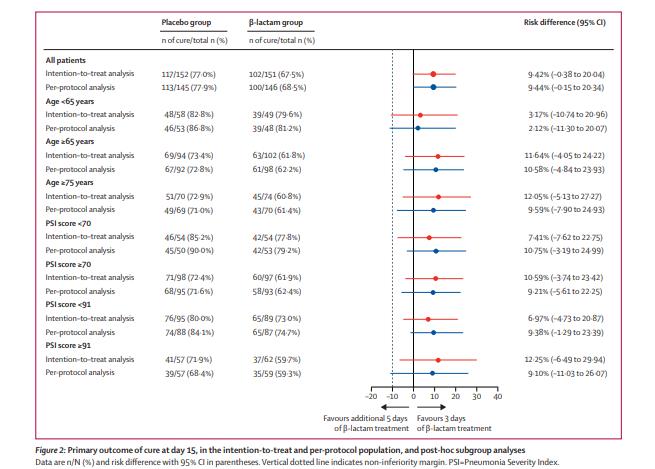
主要终点分析
研究认为,对于β-内酰胺类抗生素治疗3天后病情稳定的社区获得性肺炎住院患者,立即停药人群的预后与8天抗生素治疗人群相当。
原始出处:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#病情#
46
#Lancet#
50
#获得性#
63
#病情稳定#
76
#抗生素治疗#
77
#社区#
58
#停药#
64
学到了很多东西谢谢老师
119
顶刊就是不一样,质量很高,内容精彩!学到很多
0