Brain Connect:电导测量对老龄和阿尔兹海默症脑结构变化具有预测潜力
2021-06-01 网络 网络
电导测量具有预测潜力,特别是对年龄。虽然平均电导值显示了预期的趋势
脑白质轴突束的结构连接反映了脑的物理连接。在不同感兴趣区域之间,可以通过弥散加权磁共振成像(dMRI)测量。脑连接分析已被证明在许多条件的研究中有用,如衰老对大脑的影响,并在疾病研究。健康人群和患病人群之间大脑连接模式的差异是疾病过程导致大脑“线路”变化的潜在指标。特别是,阿尔茨海默病(AD)已被发现影响结构连通性。随着年龄的增长和AD,大脑所经历的变化可能会被混淆,从而导致AD诊断的延迟。然而,在健康老年人和AD患者中,连通性变化的时空格局是不同的。因此,对结构连接性的准确建模可能会揭示衰老和AD进展对WM退化的影响,并有助于区分两者。
Aina Frau-Pascual使用最近提出的从扩散磁共振成像中得到的结构连通性量化测量,这解释了直接和间接的途径,以量化痴呆的大脑连通性。该研究结果发表在BRAIN CONNECTIVITY杂志。
该研究分析了阿尔茨海默病神经成像计划第二阶段和成像研究开放系列数据集第三版的数据,以获得AD患者大脑变化研究的相关信息。还将这些数据集与人类连接体项目数据集进行了比较,作为参考,并最终在欧洲痴呆症DTI研究数据库的两个队列上进行了外部验证。
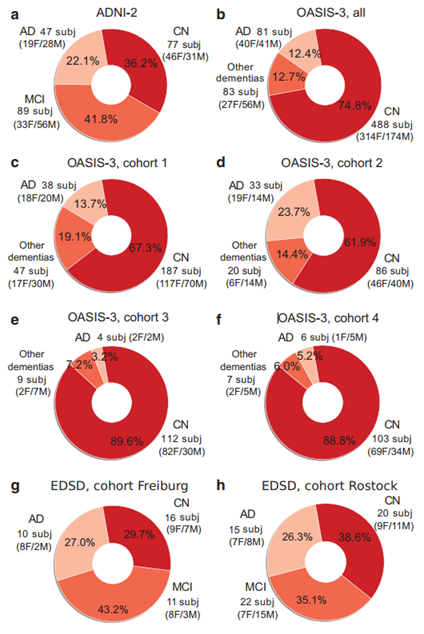
AD数据集的人口统计数据。(a) ADNI-2的213名受试者(77名认知正常, 89名MCI, 47名AD);(b) OASIS-3组652名受试者,包括4个队列,每个队列有超过100名受试者在数据表的“扫描”字段有相似的描述:(c) 272名研究对象(187名认知正常, 38名AD,47名其它痴呆),(d) 139名研究对象(86名认知正常, 33名 AD, 20名其它痴呆),(e) 125名研究对象(112名认知正常,4名AD,9名其它痴呆),以及(f) 116名研究对象(103名认知正常, 6 AD名,7名其它痴呆)。其他痴呆包括血管性痴呆,或伴有抑郁或其他症状的AD痴呆。(g) EDSD Freiburg队列(16 名认知正常, 11 MCI, 10 AD)。(h) EDSD Rostock-3T组(20名认知正常, 22名MCI, 15名AD)。
该研究分析显示了平均电导与年龄和认知得分的预期趋势,在老化数据中有显著的年龄预测值,以及以皮层下区域、扣带和颞皮质为中心的区域效应。
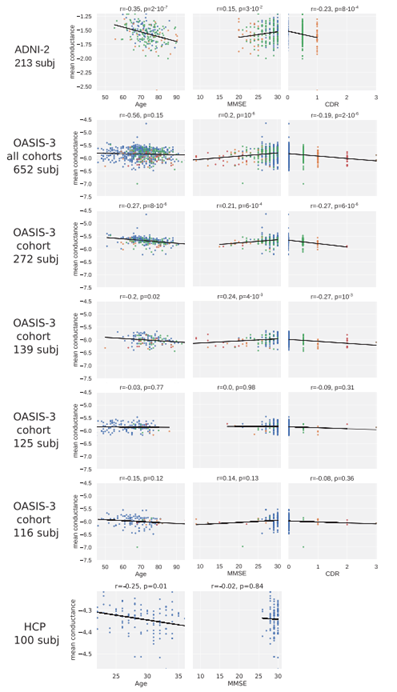
平均电导与年龄、CDR和MMSE认知得分的相关性,CDR颜色编码为0(蓝色)、0.5(绿色)、1(橙色)、2(红色)和3(棕色)。CDR不适用于HCP。
该研究将结构连通性建模为电导率,根据扩散张量给出的信息,将其计算为两个区域之间所有可能路径的加权和。该方法在产生与功能连通性更相关的结构连通性方面优于确定性径线法,这可能是因为考虑了所有路径(包括直接和间接路径)。
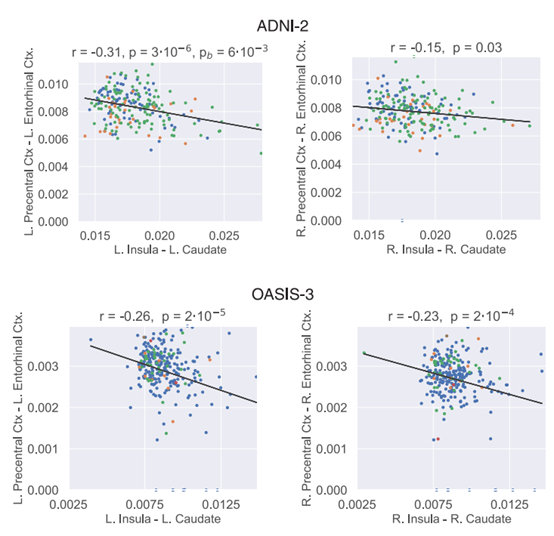
在ADNI-2(上)和OASIS-3(下)群体的272名受试者队列中,左右半球的岛叶/尾状体与中央前回/内嗅皮层结构连接呈负相关。CDR值以点的颜色编码:0(蓝色),0.5(绿色),1(橙色),2红色)和3(棕色)
该研究主要通过连接组学对老年和AD人群进行研究。将电导法应用于多个数据库,以检测与衰老和AD相关的大脑变化。结果表明,电导测量具有预测潜力,特别是对年龄。虽然平均电导值显示了预期的趋势,但认知分数的预测在不同的数据集是不同的。一个重要但并不令人惊讶的发现是,CDR和MMSE的年龄和认知分数在很大程度上是重叠的。还将不同人群之间的大脑连接相互关联起来,并发现了显著的反相关的结构连接。未来的工作包括使用纵向数据进一步探索认知分数的预测,并检验与反相关的联系确实是补偿的假设。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#NEC#
79
#阿尔兹海默#
57
#脑结构#
90
优秀
85