JOT:踝关节损伤单人复位与固定
2015-05-27 MedSci MedSci原创
背景 踝关节损伤是骨科急诊室最常见的情况之一,关于踝关节的复位和固定,有一种方法是:用弹力绷带包裹受伤的踝关节并在大腿处用胶布固定。抬高患肢使脚趾处的弹力绷带被抻长,并利用重力“自动减轻”骨折或脱位(见图1)。然而这种方法有许多局限之处,比如:不是所有的医院都有弹力绷带,就算有弹力绷带,患肢也往往因为固定不牢固而滑脱。 另一种常见的方法是让一名助手协助屈髋屈膝90°,放松小腿三头肌,方便
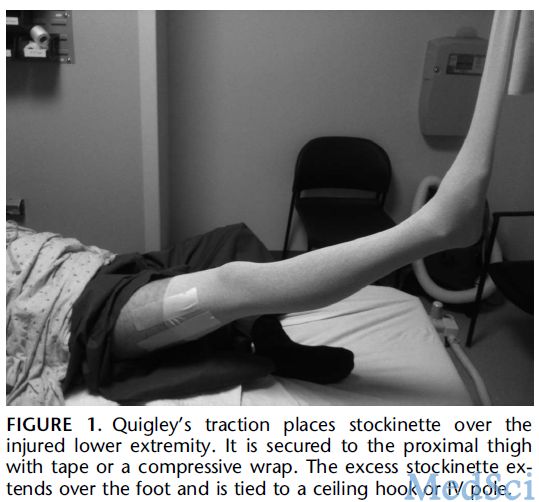
背景 踝关节损伤是骨科急诊室最常见的情况之一,关于踝关节的复位和固定,有一种方法是:用弹力绷带包裹受伤的踝关节并在大腿处用胶布固定。抬高患肢使脚趾处的弹力绷带被抻长,并利用重力“自动减轻”骨折或脱位(见图1)。然而这种方法有许多局限之处,比如:不是所有的医院都有弹力绷带,就算有弹力绷带,患肢也往往因为固定不牢固而滑脱。
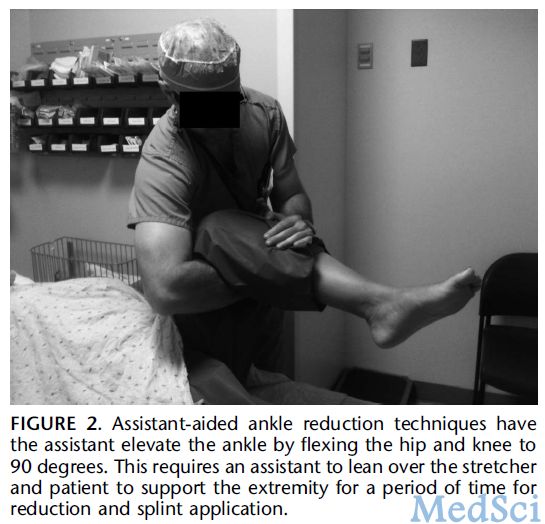
另一种常见的方法是让一名助手协助屈髋屈膝90°,放松小腿三头肌,方便操作者复位与固定踝关节。可是助手往往不熟练而无法操作到位,而且肥胖的人越来越多,“扛大腿”也越来越难(见图2)。
来自华盛顿的Nathan W. Skelley医生近日在J Orthop Trauma上介绍了一种新的方法,此法可以完全由单人操作,且不会引发严重并发症,现介绍如下。
方法
1.病人评估:对于踝关节损伤的患者,首先应该判断患肢处有无皮肤缺损、开放性骨折、烧伤或挛缩。然后进行神经血管检查。相关的影像学资料需要完善来进一步评估。本操作的禁忌包括:同侧的股骨远端骨折,胫骨平台骨折,第一及第二脚趾骨折和悬挂点附近的软组织损伤。
2.准备:患者仰卧位,操作者准备所需物品。本次操作还需要额外准备4英寸或6英寸绷带和2英寸绷带,如果有弹力绷带亦可。所有绷带至少需要1米长。第一步把绷带绕在患肢腘窝下将其吊起,嘱患者放松并拉住绷带的两端屈髋屈膝90°(见图 3)。如果是踝关节内翻损伤就将绷带两端拉过同侧肩关节,如果是外翻损伤则是对侧肩关节。最后将两端系在栏杆上,打4到6个方结。第二步悬吊患者的足部,将2英寸绷带置于足拇指与二脚趾之间,并把环结分别固定在两指的指间关节。这步的关键是固定处不要滑移,最后将两带系在输液架上使足部与膝部平行(见图 4)。可以通过调整输液架、病人和床来使踝关节处在理想的复位位置。如果操作过程中病人感到明显疼痛,应适当调整后继续。
3.复位和固定:患者体位固定后,即可通过重现损伤机制来进行复位,仅靠重力就可以维持复位(见图 5)。操作者可以有充裕的时间来准备固定。固定时操作者应站立在面对患者足底的位置,并先从足底开始包扎石膏,这样就可以实现单人操作(见图 5)。当包扎完成后,即可剪去固定膝部和拇指的绷带。
结果:作者从2011至2014年间共用此法处理51例患者,包括单、双、三踝骨折及单纯pilon骨折,效果良好,无严重并发症发生。此法简单易学,只需单人操作,应当予以推广。
原始出处:
Skelley NW1, Ricci WM.A single-person reduction and splinting technique for ankle injuries.J Orthop Trauma. 2015 Apr;29(4):e172-7. doi: 10.1097/BOT.0000000000000249.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好文,学习了
120
看看
181
#损伤#
71
#踝关节#
91