AASLD特约点评:赵明教授:Checkmate-040 研究——Nivolumab治疗晚期HCC的数据更新
2017-11-27 赵明 ioncology
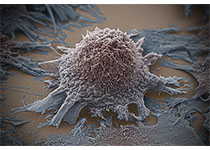
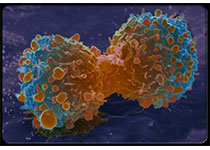
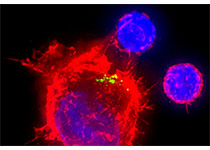
肝细胞癌(HCC)是全球第二大癌症死亡原因,每年造成近74.5万人死亡。索拉非尼作为肝细胞癌的一线全身治疗,是唯一被证明可延长总生存期的分子靶向药物,随着免疫治疗的研究进展,越来越多的数据显示PD-1拮抗剂可给晚期肝癌患者带来临床获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NIV#
101
#mAb#
71
#AASLD#
0
#Checkmate#
129
#晚期HCC#
94
#HCC#
68
#ASL#
62
非常好的文章.学习了
100