Blood:Ivosidenib或Enasidenib联合强化化疗用于新确诊的AML成人患者的疗效和安全性
2021-04-08 Nebula MedSci原创
Ivosidenib或Enasidenib联合强化化疗可改善新确诊的AML成人患者的预后
包含阿糖胞苷和蒽环类的强化诱导化疗仍是新确诊的急性髓系白血病(AML)成人患者最有效的治疗方法。近期,针对主要药物的调整改善了特定亚型患者的无事件生存期和总生存期。
异柠檬酸脱氢酶(IDH)1或2基因突变见于约20%的AML患者,突变型IDH(mIDH)蛋白催化产生D-2-羟基戊二酸(2-HG),导致DNA和组蛋白超甲基化,从而导致基因表达发生变化并影响细胞分化。
Ivosidenib(AG-120)和Enasidenib(AG-221)分别是突变型异柠檬酸脱氢酶(mIDH1)1和2酶的靶向口服小分子抑制剂。鉴于它们作为单一药物在mIDH1/2 复发性或难治性急性髓细胞性白血病(AML)中的有效性,该1期研究旨在评估Ivosidenib或Enasidenib联合强化化疗用于新确诊的mIDH1/2 AML患者的疗效和安全性。
Ivosidenib 500 mg(1/日)和Enasidenib 100 mg(1/日)在该研究条件下的耐受性良好,安全性与单独诱导和巩固化疗的安全性一致。IDH分化综合征的发生率很低,这与预期的同时进行细胞毒性化学疗的情况一样。
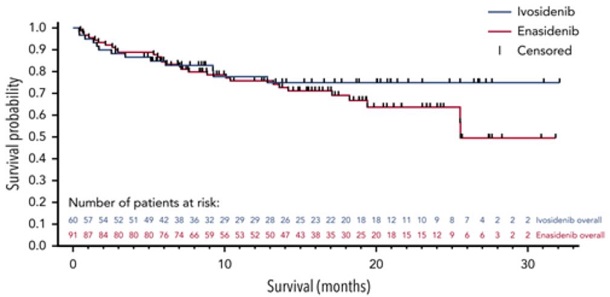
总存活率
在接受Ivosidenib+强化化疗的患者中,QT间期延长的频率和等级与Ivosidenib单药治疗时所观察到的相似。在接受Enasidenib治疗的患者中,总胆红素升高的频率更高,这与该抑制剂已知的抑制UGT1A1的潜力相符,但似乎没有重大意义的临床结果。
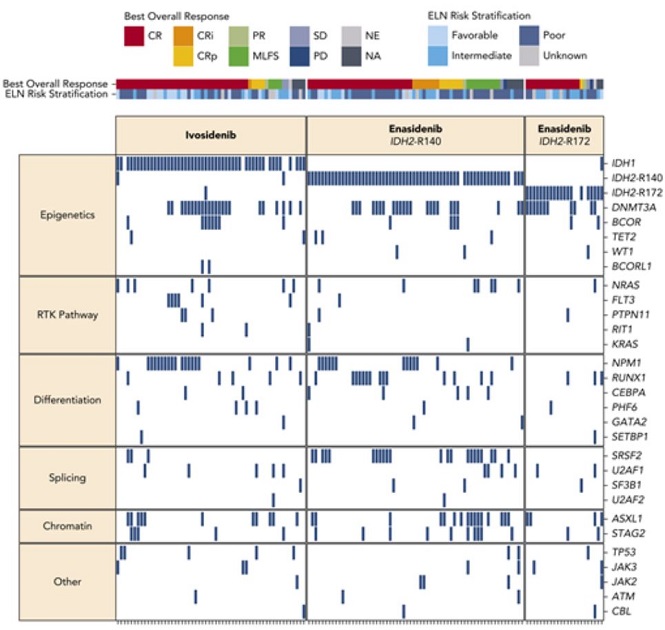
基础突变谱和最佳总临床反应
在接受Ivosidenib(n=60)或Enasidenib(n=91)的患者中,诱导后完全缓解率分别为55%和47%,CR/CR伴不完全中性粒细胞或血小板恢复(CR/CRi/CRp)率分别为72%和63%。
在CR/CRi/CRp总体反应最佳的患者中,Ivosidenib组中有16/41(39%)位患者获得了IDH1突变清除,而Enasidenib组中有15/64(23%)位获得了IDH2突变清除(PCR);此外,分别还有16/20(80%)和10/16(63%)位患者的可检测的残留疾病转为了阴性(多参数流失细胞术)。
总而言之,Ivosidenib或Enasidenib联合强化化疗可改善新确诊的mIDH1/2 AML成人患者的预后。
原始出处:
Eytan M. Stein, et al. Ivosidenib or enasidenib combined with intensive chemotherapy in patients with newly diagnosed AML: a phase 1 study. Blood (2021) 137 (13): 1792–1803. https://doi.org/10.1182/blood.2020007233
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Ivosidenib#
75
#疗效和安全性#
63
已读,真是受益匪浅呀!
0
谢谢梅斯提供这么好的信息,学到很多
77
学习了
90
学到了
84