心脏瓣膜手术-正常解剖、手术适应症、手术过程和手术预后(图片)
2015-12-02 网络 MedSci原创
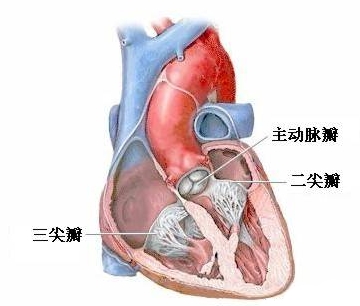
心脏有四个瓣膜:主动脉瓣、二尖瓣、三尖瓣和肺动脉瓣。瓣膜的作用是控制血液在心脏的流动方向。心脏瓣膜的打开与关闭就产生心音。 心脏瓣膜置换术适应症有: *心脏瓣膜狭窄 *心脏瓣膜漏 心脏瓣膜疾病可以由风湿热和感染性心内膜炎引起。手术需要对病人进行全身麻醉,手术切口在胸部胸骨正中线。

心脏有四个瓣膜:主动脉瓣、二尖瓣、三尖瓣和肺动脉瓣。瓣膜的作用是控制血液在心脏的流动方向。心脏瓣膜的打开与关闭就产生心音。

心脏瓣膜置换术适应症有:
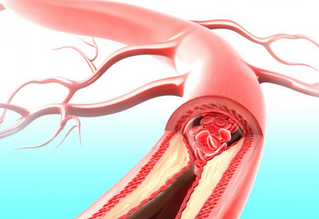
*心脏瓣膜狭窄
*心脏瓣膜漏
心脏瓣膜疾病可以由风湿热和感染性心内膜炎引起。手术需要对病人进行全身麻醉,手术切口在胸部胸骨正中线。

心脏瓣膜手术属开胸手术。手术过程中,中断心脏的血液供应,病人的血液通过人工管道被输送到心肺旁路装置,这装置暂时代替病人的心肺功能,维持血液的正常氧化和循环。
瓣膜可以修复也可以置换。用于置换的瓣膜可以是生物瓣膜或人工瓣膜。生物瓣膜来自捐赠者尸体,经修整的生物瓣膜来自动物供体(通常是猪),人工瓣膜用金属或塑胶制成。置换生物瓣膜的病人术后很少需要终生服用抗凝剂。

心脏瓣膜置换术的手术成功率正不断地上升。术后病人症状缓解,生命得到延长。死亡率取决于原心脏瓣膜情况,平均为2%-5%。
大约有70%置换人工二尖瓣的病人术后可存活9年。这些置换了人工心脏瓣膜的病人需要终生服用抗凝剂,而且,可以在病人的胸部听到心脏跳动时人工瓣膜发出的金属样的“滴答”声,这是正常现象。
心脏瓣膜置换术后的病人要住在深切治疗室2-3天,监视心脏功能。术后平均住院时间为3周。完全康复需要数周至数月的时间,视病人手术前的健康情况而定。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#瓣膜手术#
91
#正常解剖#
70
#心脏瓣膜#
72
好文章,值得收藏
50
#适应症#
73
#瓣膜#
67