Eur Heart J :迷走神经刺激的低射血分数心衰治疗研究
2015-02-23 张旭栋 MedSci原创
增加交感神经激活和降低副交感神经兴奋性,其反映减少的压力反射敏感性和/或降低的心脏心率变异性,不论病因的进展,都对心脏衰竭(HF)患者有潜在重要的病理生理贡献,而且与预后不良有关。副交感神经兴奋性增强在心衰进展中,具有潜在的自主神经功能失调和抑制作用。目前,对于左心室收缩功能障碍的非随机实验研究中,通过直接刺激迷走神经从而增强副交感神经兴奋性,其结果提示迷走神经对生活质量,运动能力,以及左心室重塑
增加交感神经激活和降低副交感神经兴奋性,其反映减少的压力反射敏感性和/或降低的心脏心率变异性,不论病因的进展,都对心脏衰竭(HF)患者有潜在重要的病理生理贡献,而且与预后不良有关。副交感神经兴奋性增强在心衰进展中,具有潜在的自主神经功能失调和抑制作用。目前,对于左心室收缩功能障碍的非随机实验研究中,通过直接刺激迷走神经从而增强副交感神经兴奋性,其结果提示迷走神经对生活质量,运动能力,以及左心室重塑有改善。法国洛林大学,南锡大学中心医院心内科 Faiez Zannad等人,通过NECTAR-HF实验随机、假对照试验评估刺激迷走神经安全性,以及能否延缓心脏重塑,改善心脏功能,并增加运动能力,提高生活质量。成果发表在2月份European heart journal期刊上。
目的:心脏衰竭的神经心脏治疗(NECTAR-HF)(一项随机、假对照试验),旨在评估有严重左心室收缩功能障碍症状的心衰患者,单剂量的迷走神经刺激(VNS)是否会延缓心脏重塑,改善心脏功能,并增加运动能力。
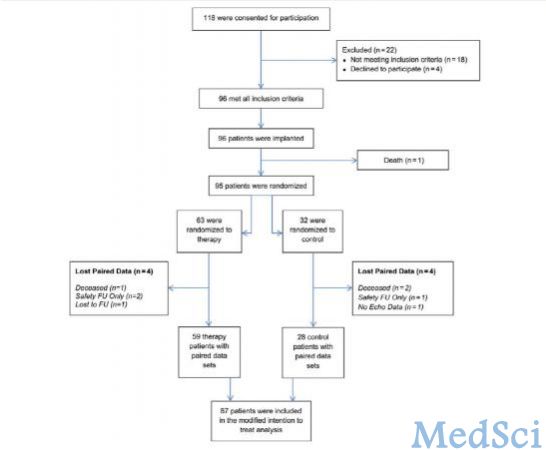
方法:患者被随机分为治疗组(迷走神经刺激)或对照组(没有迷走神经刺激),比例为2:1,进行为期6个月试验。主要终点是6个月后,对照组与治疗组相比,左心室收缩末期内径(LVESD)的变化,其次要终点为超声心动图测量,运动能力,生活质量的评估,24小时动态心电图,以及循环生物标志物。
结果:96例植入患者中,87例配对主要终点。6个月后,治疗组LVESD基线水平变化为-0.04±0.25厘米,对照组LVESD基线水平变化为-0.08±0.32厘米(P=0.60)。左心室舒张末期内径,左室收缩末期容积,左室舒张末容积,左室射血分数,峰值V02,和N终端脑钠素前体,超声心动图参数相比于对照组而言,没有表现出优势。然而,治疗组显示有显著统计学意义,分别是明尼苏达州心力衰竭生活质量问卷(P = 0.049),纽约心脏学会心功能分级(P =0.032),和SF-36量表(P = 0.016)。
结局: 虽然NECTAR-HF试验迷走神经刺激未能证明其对有症状的心衰患者主要和次要终点(心脏重塑和功能)有改善,但生活质量却有了显著的改善。
原文出处:
Zannad F, De Ferrari GM, Tuinenburg AE, Wright D, Brugada J, Butter C, Klein H, Stolen C, Meyer S, Stein KM, Ramuzat A, Schubert B, Daum D, Neuzil P, Botman C, Castel MA, D'Onofrio A, Solomon SD, Wold N, Ruble SB. Chronic vagal stimulation for the treatment of low ejection fraction heart failure: results of the NEural Cardiac TherApy foR Heart Failure (NECTAR-HF) randomized controlled trial. European heart journal. 2015;36(7):425-33.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#低射血分数#
68
#ART#
55
#神经刺激#
62
#HEART#
60
不错,不错!
183