CORR:OA患者关节置换术后身体活动水平并无提高
2014-05-27 佚名 丁香园
老年骨性关节将导致患者关节疼痛和功能障碍,影响患者的日常及工作活动。全髋、全膝关节置换可以迅速缓解疼痛、改善肢体功能,提高生活质量。但是关节置换术后患者的的身体活动情况在术后能否得到提高却一直没有明确的研究。【原文下载】 针对上述问题,澳大利亚的Paula Harding D医生首次使用GT1M加速器对全髋全膝关节置换患者的身体活动情况进行了一项研究,发现骨性关节炎患者进行关节置换术后患者客
老年骨性关节将导致患者关节疼痛和功能障碍,影响患者的日常及工作活动。全髋、全膝关节置换可以迅速缓解疼痛、改善肢体功能,提高生活质量。但是关节置换术后患者的的身体活动情况在术后能否得到提高却一直没有明确的研究。【原文下载】
针对上述问题,澳大利亚的Paula Harding D医生首次使用GT1M加速器对全髋全膝关节置换患者的身体活动情况进行了一项研究,发现骨性关节炎患者进行关节置换术后患者客观上的身体活动情况并未有明显改善,患者在术前和术后均喜欢久坐,其体力活动能力并没有达到美国国民体育运动健身指南中建议的标准,其结果发表在2014年5月的 Clinical Orthopaedics and Related Research杂志上。
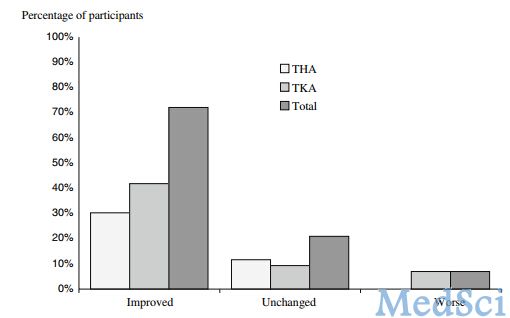
57例老年骨性关节炎接受关节置换的患者进入研究,所有患者在关节置换术前无需乘坐轮椅可自由活动并且没有脑中风及认知障碍,其中33例患者进行全膝关节置换,24例进行全髋关节置换。有44例患者完成整个随访及检查。
患者在关节置换术后进行标准的物理治疗,包括术后1天在助行器及理疗师帮助下开始负重行走,并进行床上运动练习。使用GT1M加速器测量患者术前及术后6个月时的运动情况,并对患者疼痛、髋膝关节评分、生活质量等情况进行评估和分析。
患者在关节置换术前一天中有82%的时间是坐着不动的,一部分人自述有时参加散步、有限的购物等轻度活动。在术后6个月时,接受全髋置换或全膝关节置换的患者通过GT1M加速器客观测量到的体力运动情况和术前并未有明显改变,一天中有83%的时间患者是坐着不动的。
在关节置换术前,57例患者中只有3例患者的体力运动达到美国国民体育运动健身指南对于身体活动的要求,而在术后6个月时,资料完整的52例患者中只有1例全髋关节置换的患者能够达到健身指南要求。
因此作者建议医生调整治疗及康复方案以提高关节置换患者的身体活动能力改善其健康水平,需要对影响关节置换术后的身体活动水平的因素进行进一步的研究。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#关节置换术#
55
#置换#
66
#身体活动#
53
#置换术#
53
#ORR#
62