本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
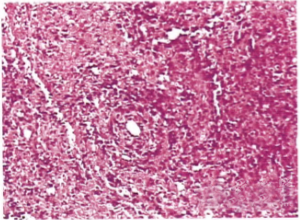

图 T2WI磁共振影像[ A(左):右侧肾上腺肿瘤 B(右):左侧肾上腺肿瘤 ] 病例摘要 患者,男性,64岁,高血压20余年,3个月前出现头晕、肢体无力、周期性麻痹,昼间尿量800 ml,夜间尿量1000 ml。 血压为200/110 mmHg,血钾为2.4 mmo
原发性肝癌是目前我国第四位的常见恶性肿瘤及第三位的肿瘤致死病因,严重威胁我国人民的生命和健康1,2。原发性肝癌主要包括肝细胞癌(Hepatocellular Carcinoma,HCC)、肝内胆管癌(Intrahepatic Cholangiocarcinoma,ICC)和HCC-ICC混合型三种不同病理类型,三者在发病机制、生物学行为、组织学形态、治疗方法以及预后等方面差异较大,其中肝细胞癌占到
最常见的心脏原发性恶性肿瘤是肉瘤,其又分为血管肉瘤、横纹肌肉瘤、纤维肉瘤、平滑肌肉瘤等。它们各自有何特点?
手部X线显示左中、右小指远节指骨为溶骨性病变(如图所示)。最近的PET扫描显示无胸外疾病。在缺乏创伤或感染的情况下,该患者被诊断为原发性肺癌溶骨性转移瘤,在左中指末节截肢后经组织学予以证实。术后功能良好,手指无持续疼痛。医务人员采用镇痛治疗右手小指。该患者几个月后死于原发疾病。
2017年10月,发表在《Chest》的一项由美国科学家进行的研究考察了氯法齐明治疗原发性和难治性非结核分枝杆菌(NTM)感染的安全性和有效性。
原发性胆汁性胆管炎(PBC)是一种异质性相对较强的疾病,不同患者的临床经过及表型可能存在较大差异。因此,必须给予长期的治疗和随访才能对患者进行准确的危险分层


梅斯医学MedSci APP
医路相伴,成就大医
#原发性#
55
#视网膜#
45
#玻璃体#
48
很好
97