Mov Disord:神经丝轻链可预测多发性系统萎缩的疾病严重程度和进展
2021-11-04 MedSci原创 MedSci原创
线血浆NFL水平与MSA患者的运动严重程度和进展显著相关(P<0.05),但与认知进展无关(P>0.05)。血浆NFL是MSA疾病严重程度和监测MSA进展的可靠生物标志物。
多系统萎缩(MSA)是一种罕见的成人发作的进行性神经退行性疾病,其特征是自主神经功能衰竭、帕金森病、小脑共济失调和锥体体征的可变组合。MSA进展迅速,且没有有效的治疗方法;中位生存时间约为6至10年。迫切需要能够预测MSA进展的生物标志物。神经丝轻链(NFL)作为神经退行性疾病中轴突损伤的候选生物标记物,不仅在脑脊液(CSF)中,而且在血清中也越来越受到重视。MSA患者血浆NFL水平高于帕金森病患者和健康对照组(HCs)。然而,目前缺乏关于NFL水平与MSA严重程度和进展之间关系的研究。
华西医院Huifang Shang等在Mov Disord杂志发表研究文章,检测了MSA患者血浆NFL水平,以研究血浆NFL水平是否与MSA严重程度相关,并阐明血浆NFL与MSA进展之间的关系,探讨血浆NFL水平是否与MSA患者的运动和认知功能进展相关。
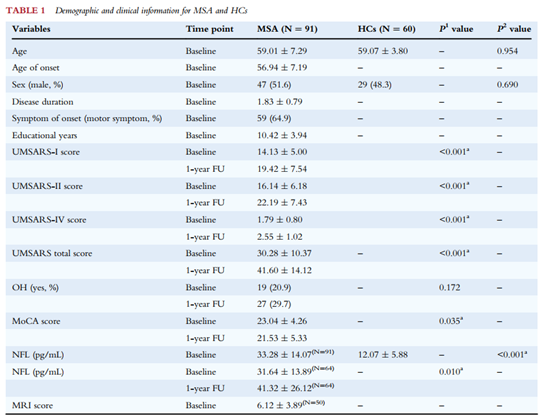
共纳入91例MSA患者和60名健康对照者(HCs)。MSA患者血浆NFL水平在基线时显著高于HCs(P<0.001)。64例MSA患者的NFL水平从基线上升到随访1年(P = 0.010)
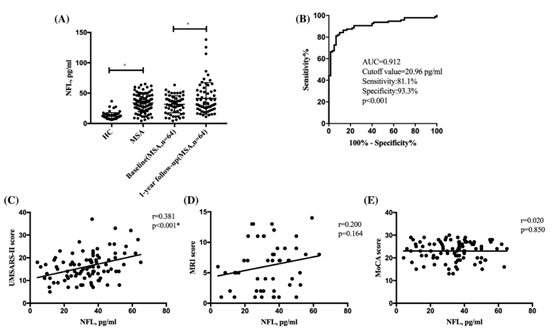
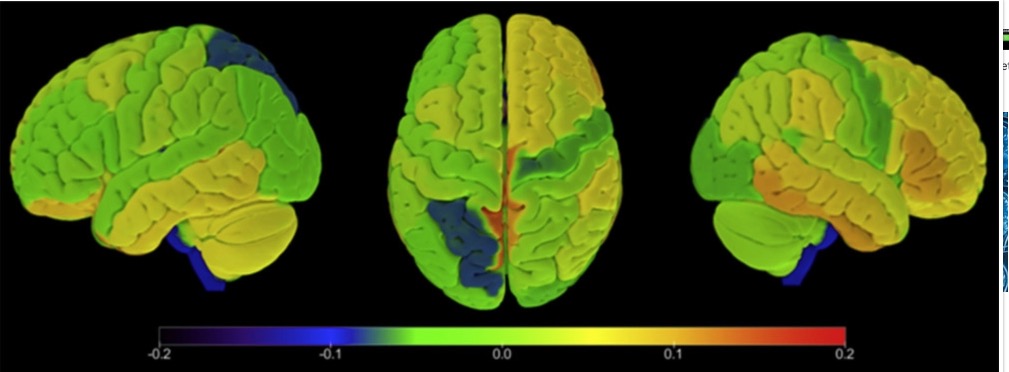
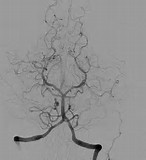
不同组的血浆神经丝轻链(NFL)水平及其与疾病严重程度的相关性。(A) 多系统萎缩(MSA)患者与健康对照者(HCs)之间血浆NFL水平的比较,以及64例MSA患者基线检查与1年随访之间血浆NFL水平的比较。(B) ROC分析,以区分MSA和HCs。(C) 基线血浆NFL水平与统一MSA评分量表II得分之间的相关性。(D)基线血浆NFL水平与MRI评分之间的相关性。(E)基线血浆NFL水平与蒙特利尔认知评估得分之间的相关性。
受试者操作特征曲线(ROC)分析用于评估血浆NFL区分MSA和HCs患者的能力。结果表明,血浆NFL截止值为20.96 pg/mL时,敏感性为81.1%,特异性为93.3%,曲线下面积为0.912(图1B)。基线NFL水平与MSA患者的UMSARS-II评分显著相关(P<0.001)。然而,基线NFL水平与MSA患者的MoCA和MRI得分之间没有相关性(P>0.05)。(图1C、D、E)。基线血浆NFL水平与MSA患者的运动进展显著相关(β=0.296,SE=0.043,P=0.009)(在调整年龄、性别、病程、诊断亚型、OH和基线UMSARS评分后),但与认知进展无关(β=0.071,SE=0.026,P=0.306)(调整年龄、性别、病程、诊断亚型、OH、教育年限和基线MoCA得分后)
综上所述,基线血浆NFL水平与MSA患者的运动严重程度和进展显著相关(P<0.05),但与认知进展无关(P>0.05)。血浆NFL是MSA疾病严重程度和监测MSA进展的可靠生物标志物。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Dis#
52
#Disord#
61
#萎缩#
62
#神经丝轻链#
102
#多发性#
61
#神经丝#
55