Clin Gastroenterology H:回盲部切除术后内镜下缓解患者克罗恩病术后晚期复发的风险分析
2021-06-13 MedSci原创 MedSci原创
克罗恩病(CD)是一种慢性致残性炎症性肠病(IBD),大约一半的病人在确诊后的头十年需要手术治疗,三分之一的患者在病程中需要多次进行肠切除手术。
克罗恩病(CD)是一种慢性致残性炎症性肠病(IBD),大约一半的病人在确诊后的头十年需要手术治疗,三分之一的患者在病程中需要多次进行肠切除手术。Rutgeerts评分可以对回盲部切除术后内镜下CD复发症状的严重程度进行分级,从而判断内镜下疾病复发情况。一般来说,Rutgeerts评分i0(无内窥镜病变)或i1(新末端回肠1至5处阿弗他病变)反映内窥镜病情缓解,但是早期内窥镜病情缓解并不排除长期疾病并不会复发。因此,本项研究对克罗恩病(CD)术后1-10年复发的风险进行了相关研究。

研究人员在法国和比利时的3个炎症性肠病(IBD)中心进行了一项回顾性研究,试验进行的时间从2006年开始到2016年结束,所有CD患者(n=86)都接受了回盲部切除术,在基线评估时没有内窥镜证据显示疾病存在复发(Rutgeerts评分低于i2)。基线内窥镜检查后的术后复发被定义为至少达到以下1项:临床复发、IBD相关的住院治疗、肠损伤的发生、需要内窥镜行球囊扩张吻合口以及需要重复手术治疗。
手术和基线内镜检查之间的中位时间为7个月(IQR,5.7-9.5个月);40例(46.5%)在此期间接受了药物预防。35名患者(40.7%)出现术后晚期复发,基线内镜检查后疾病复发的中位时间为14.2个月(IQR,6.3–26.1个月)。在基线检查时,Rutgeerts评分为i0(20/55)或i1(15/31)的患者的复发状态没有显著差异(P=0.28),并且与药物预防无关(预防性治疗组16/40,未预防性治疗组19/46;P=0.90)。同时,71例患者中有29例(40.8%)存在粘膜损伤病变进展。
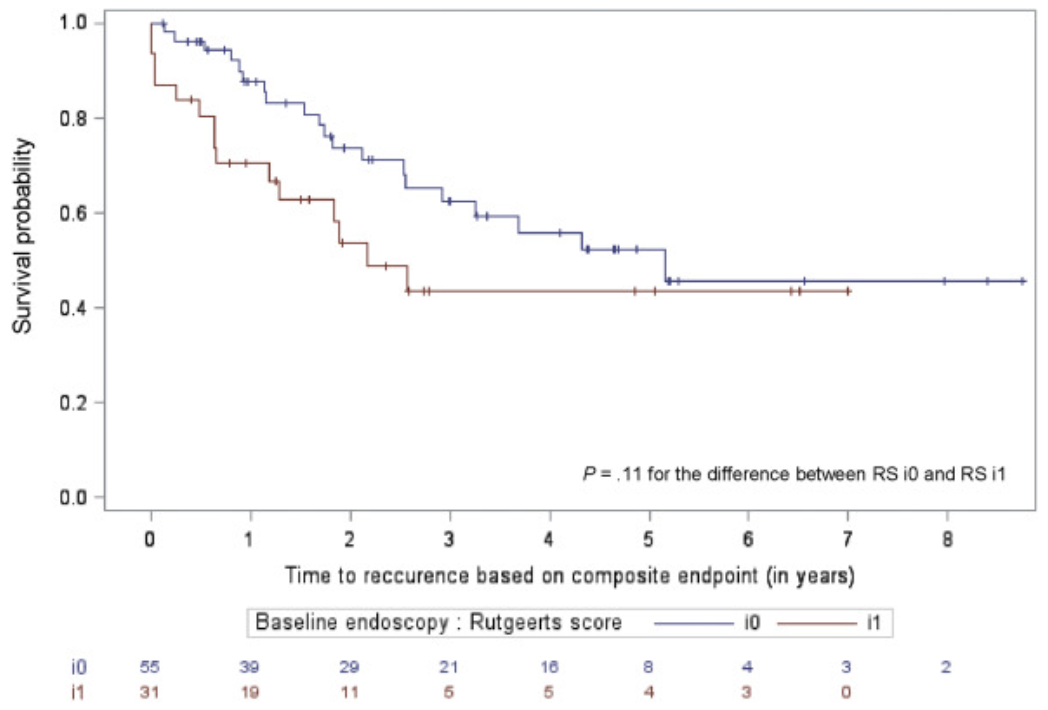
图:回盲部切除术后内镜下缓解患者克罗恩病术后晚期复发的表现
本项研究发现在回盲部切除术治疗的CD患者中,40%的患者在中位随访时间为3.5年后出现晚期复发,尽管最初的有内镜下缓解,但仍建议在18个月后对这些患者进行严密疾病活动度监测。
原始出处:
Lieven Pouillon. Et al. Risk of Late Postoperative Recurrence of Crohn’s Disease in Patients in Endoscopic Remission After Ileocecal Resection, Over 10 Years at Multiple Centers. Clinical Gastroenterology and Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
60
#GAS#
46
#切除术#
53
#AST#
66
#内镜#
68
#Gastroenterology#
65
不错,学习了
84