JTO:吉非替尼同步胸腔放疗治疗不可切除的EGFR突变局部晚期非小细胞肺癌
2021-06-26 MedSci原创 MedSci原创
约 10% 的局部晚期非小细胞肺癌 (LA-NSCLC) 患者伴有表皮生长因子受体 (EGFR) 突变。这部分患者对免疫检查点抑制剂不敏感,EGFR-酪氨酸激酶抑制剂 (TKI) 仍然是目前主要治疗措
约 10% 的局部晚期非小细胞肺癌 (LA-NSCLC) 患者伴有表皮生长因子受体 (EGFR) 突变。这部分患者对免疫检查点抑制剂不敏感,EGFR-酪氨酸激酶抑制剂 (TKI) 仍然是目前主要治疗措施。
本研究招募了具有敏感 EGFR 突变(外显子 19 缺失或外显子 21 L858R 点突变)的未接受化疗、不可切除的 LA-NSCLC 患者。患者接受吉非替尼(250mg/天,持续 2 年)加同步 TRT(64Gy/32frs)治疗。主要终点是 2 年的无进展生存期 (PFS)(试验号,UMIN000008366)。
2012 年 8 月至 2017 年 11 月期间,共有 28 名患者入组,27 名符合条件。中位年龄为 67 岁;从不/现在或以前吸烟者 15 / 12;ECOG 表现状态 0 / 1 19 / 8;EGFR 外显子 19 缺失 / 外显子 21 L858R 13 / 14;和 c 阶段 IIIA / IIIB 14 / 13。独立审查的两年 PFS 率为 29.6%。ORR 为 81.5%,中位 PFS 为 18.6 个月,中位 OS 为 61.1 个月。大约一半的患者表现为孤立性脑转移作为他们的第一个复发部位。≥ 3 级的不良事件包括疲劳、皮肤反应和食欲减退(各 3.7%)。
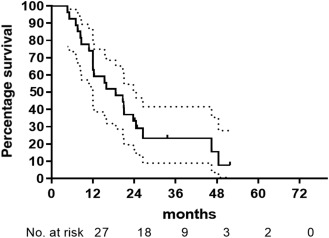
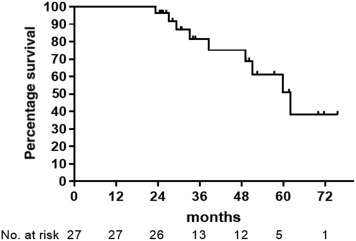
这项前瞻性研究显示了吉非替尼联合同步 TRT 在 EGFR 突变的局部晚期NSCLC 患者中的耐受性和可能的疗效。这项前瞻性研究揭示了吉非替尼联合同步 TRT 对具有敏感 EGFR 突变的 LA-NSCLC 患者的耐受性和可能的疗效。 结合 EGFR TKI 用于局部晚期疾病的进一步研究是有必要的,并且可以使用具有中枢神经系统活性的药物进一步改善结果。 此外,探索最佳给药方式对于将结果推广到临床实践也很重要。
原始出处:
Akamatsu H, Murakami H, Harada H, Shimizu J, Hayashi H, Daga H, Hasegawa Y, Kim YH, Kato T, Tokunaga S, Nishimura Y, Yamamoto N, Nakagawa K, Gefitinib with concurrent thoracic radiotherapy in unresectable locally advanced non-small cell lung cancer with EGFR mutation; West Japan Oncology Group 6911L, Journal of Thoracic Oncology (2021), doi: https://doi.org/10.1016/j.jtho.2021.05.019.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#局部晚期#
46
#非小细胞#
0
赞
84
#局部#
48
#GFR#
0
有用
62