Euro Radio:LI-RADS虽好,但一定要用对哦!
2022-03-04 shaosai MedSci原创
据调查,肝癌是全球癌症相关死亡的第四大常见原因。超声检查(US)、磁共振成像(MRI)和计算机断层扫描(CT)等成像方式在肝癌高风险患者的监测、早期诊断、分期和治疗反应评估中发挥了重要作用。
 据调查,肝癌是全球癌症相关死亡的第四大常见原因。超声检查(US)、磁共振成像(MRI)和计算机断层扫描(CT)等成像方式在肝癌高风险患者的监测、早期诊断、分期和治疗反应评估中发挥了重要作用。
据调查,肝癌是全球癌症相关死亡的第四大常见原因。超声检查(US)、磁共振成像(MRI)和计算机断层扫描(CT)等成像方式在肝癌高风险患者的监测、早期诊断、分期和治疗反应评估中发挥了重要作用。
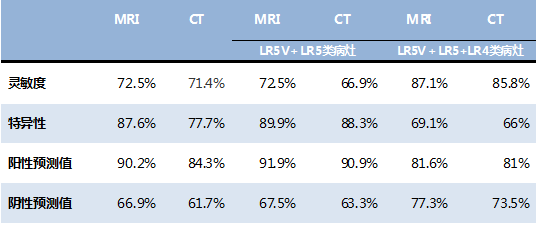
由美国放射学会(ACR)提出的肝脏成像报告和数据系统(LI- RADS,LR),为肝细胞癌(HCC)成像提供了标准化的术语、技术、解释和报告。LI-RADS CT/MRI诊断算法为高危患者的肝癌筛查提供了分类参考,其中每个类别反映了良性、恶性和HCC的概率。LR-3(中等恶性概率)、LR-4(可能HCC)和LR-5(明确的HCC)类别是根据五个主要特征的组合来分配的:非边缘动脉期高强化(APHE)、非边缘廓清(以下简称WO)、包膜强化(以下简称囊)、大小和阈值增长(TG)。
与大多数其他恶性肿瘤不同,HCC的明确诊断通常是基于影像学,而且在治疗(包括肝移植)之前无需进行组织学确认。因此,LR-5成像标准的目标是为HCC的诊断提供100%的特异性。
然而现阶段,临床上对LI-RADS的表现知之甚少,在临床实践中多种因素可能影响病例的解释和报告。近日,发表在European Radiology杂志的一项研究评估了临床上使用LI-RADS v2017或v2018报告的不符合LR-5标准的LR-5比例,以了解LR-5标准错误应用的频率并分析这些错误的原因,为提高LI-RADS分类的诊断性能提供了指导。
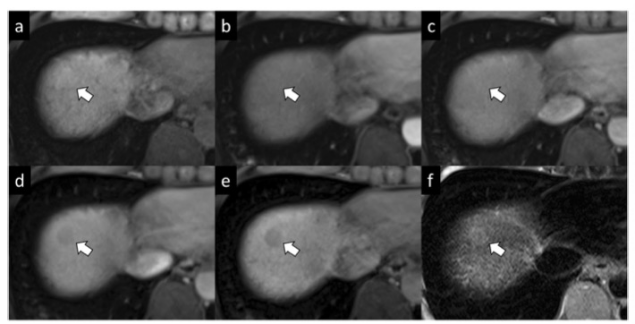
本项研究于2017年4月至2020年9月期间使用标准化LI-RADS模板回顾了的所有本机构的MR和CT报告。对于每个报告的LR-5提取了尺寸、主要征象(MFs)和LI-RADS版本(v2017或v2018)的分级。报告的MF被用来确定是否使用LI-RADS的应用版本满足LR-5标准,并对数据进行了描述性的总结。
其中,有234名患者(67.6%为男性,平均年龄66.2岁)的38个病变结果被认定为LR-5,包括136个(44.2%)v2017版和172个(55.8%)v2018版。有8/136(6%)v2017版LR-5和6/172(3%)v2018版LR-5不符合LR-5标准。在8个错误分类的v2017中,3个(43%)缺乏APHE,1个(14%)是只有APHE的16毫米的新病变,4个(43%)是10-19毫米的具有APHE和WO的病变。在6个错误分类的v2018中,5个(83%)缺乏APHE,1个(17%)<10毫米。
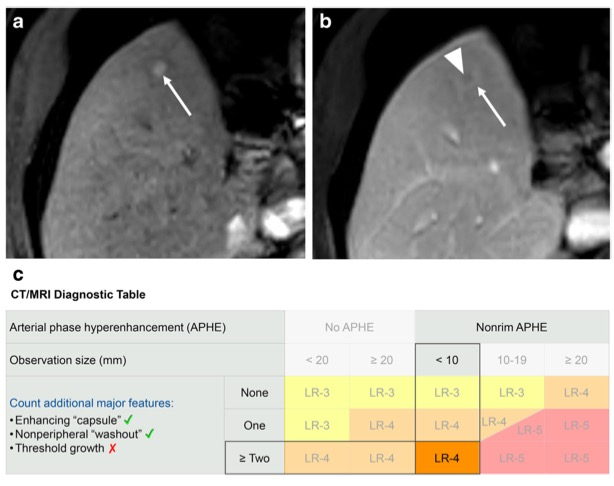
图 一名57岁丙型肝炎肝硬化男性患者的分类结果。病变(箭头)被判定为有非边缘动脉期的高强化(a)、非边缘的廓清(箭头,b)和一个强化的包膜(箭头,b)。其大小为9毫米。根据LI-RADS v2018,该观察结果被分类为LR-5,但使用LI-RADS v2018 CT/MRI诊断表的正确类别是LR-4。
总之,根据LI-RADS的分类标准,临床实践中报告的3-7%的LR-5病变不符合基于报告的主要成像特征的LR-5标准,因此进一步的影像学征象的准确识别将助于减少这些报告错误的频率并挺高诊断准确性。
原文出处:
Maryam Ghadimi,Jason Birnbaum,Ihab R Kamel,et al.What proportion of LI-RADS 5 observations reported in clinical practice do not meet LI-RADS 5 criteria?.DOI:10.1007/s00330-021-08389-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ADS#
99
#LI-RADS#
94
#PE#
80
#RADS#
83