Diabetologia:无缺失癌胚抗原相关细胞粘附分子2的雄性小鼠中年龄依赖性胰岛素抵抗如何?
2017-09-30 MedSci MedSci原创
近日,国际杂志 《Diabetologia》上在线发表一项关于无缺失癌胚抗原相关细胞粘附分子2基因的雄性小鼠中年龄依赖性胰岛素抵抗的研究。
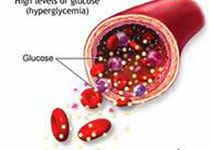
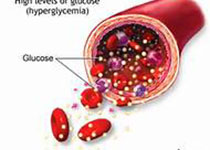
近日,国际杂志 《Diabetologia》上在线发表一项关于无缺失癌胚抗原相关细胞粘附分子2基因的雄性小鼠中年龄依赖性胰岛素抵抗的研究。 缺乏编码癌胚抗原相关细胞粘附分子2(Cc2 [也称为Ceacam2 ])基因的Cc2-/-小鼠表现食欲增加,并导致肥胖和胰岛素抵抗。这在雌性小鼠的2个月龄开始发生。由于对白色脂肪组织的交感神经紧张和能量消耗增加,直到最后一次检查(7-8个月),雄性突变体维持正常的体重和胰岛素敏感性。目前的研究旨在调查在成年后的突变雄鼠体内的胰岛素抵抗是否会随着胰岛素体内平衡的变化而发生变化。 研究通过胰岛素和葡萄糖耐量试验评估胰岛素反应。通过间接测热法分析能量平衡。雄性Cc2-/-小鼠在约9个月龄时发现明显的代谢异常。这些包括升高的总脂肪量,高胰岛素血症和胰岛素抵抗(由葡萄糖和胰岛素不耐受确定,喂食高血糖和降低的胰岛素信号通路)。配对实验表明,胰岛素抵抗是由食欲过多引起的。间接量热法证明老年突变体雄性小鼠损害了能量消耗。尽管由Cc2缺失引起的胰岛素分泌增加,但在突变雄性小鼠中,直到大约9个月大的时候,慢性高胰岛素血症并没有发展,此时胰岛素清除率开始显著下降。这可能
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
60
#BET#
51
#胰岛#
58
#癌胚抗原#
62
#抗原#
51
已学习.值得分享!
72
好资料学习了!
104
学习了受益匪浅
97