反式肩关节置换治疗陈旧性肱骨近端骨折伴肱骨头缺如1例
2019-09-12 谢尚举 曹国平 全仁夫 中国骨伤
患者,女,48岁,因左肩关节疼痛伴活动不利3年余,加重2个月入院。患者3年前因外伤致左肱骨近端粉碎性骨折,当时因要求保守治疗未及时手术。3年来左肩关节间歇性疼痛,症状时轻时重,活动时疼痛加重,长期服用非甾体类镇痛药物缓解症状。左肩关节外观畸形,功能基本丧失,无法完成前臂抬举、梳头、进食等基本生活动作。后曾至多家医院就诊,均建议行肩关节置换手术治疗。近2个月来患者因轻度外伤致左肩关节疼痛加剧,左上肢
临床资料
患者,女,48岁,因左肩关节疼痛伴活动不利3年余,加重2个月入院。患者3年前因外伤致左肱骨近端粉碎性骨折,当时因要求保守治疗未及时手术。3年来左肩关节间歇性疼痛,症状时轻时重,活动时疼痛加重,长期服用非甾体类镇痛药物缓解症状。左肩关节外观畸形,功能基本丧失,无法完成前臂抬举、梳头、进食等基本生活动作。后曾至多家医院就诊,均建议行肩关节置换手术治疗。近2个月来患者因轻度外伤致左肩关节疼痛加剧,左上肢活动明显受限,静息时易感疼痛,影响正常睡眠,遂来我院就诊。患者既往有先天性脊柱侧弯病史;高血压及糖尿病10余年,平时血压及血糖控制尚可。素来无重体力劳动,无吸烟饮酒等不良嗜好。入院查体:脊柱侧弯,双上肢无明显感觉麻木;左肩关节压痛阳性,左肩关节活动异常;左肩落臂试验阳性,拿破仑试验阳性,外旋抗阻试验阳性,左肩主动活动前屈40°,外展30°,后伸20°;左侧三角肌肌力Ⅳ,右侧三角肌肌力正常。影像学检查,左肩X线片(图1a)示左肱骨近端陈旧性骨折,左肱骨头坏死。左肩CT及三维重建(图1b,1c,1d,1e)示左肱骨近端骨缺损,左肱骨头缺如,左肩胛盂下角陈旧性骨折。左肩MRI(图1f,1g)示左肩袖结构缺损,左肩关节结构紊乱,左肩关节积液。实验室检查:红细胞128g/L,白细胞6.67×109/L,血小板97×109/L,C-反应蛋白(CRP)3.4mg/L,血沉(ESR)21mm/h,余无特殊异常指标。结合患者病史及实验室检查,临床诊断为:左肱骨近端陈旧性骨折;左肱骨头坏死,左肩袖缺损。

患者首要治疗诉求为缓解左肩关节疼痛,并尽可能恢复左肩关节外形及基本功能。告知患者及家属通过左肩关节融合或钢板内固定的手术方式可能无法完全解除左肩疼痛,仍需长期服用镇痛药物治疗。若采取左侧半肩关节置换,由于肩袖挛缩明显,术中无法修复,术后功能恢复较差,左上肢抬举及旋转活动仍困难。若采取反式肩关节置换,可较大程度缓解左肩疼痛并有望通过术后康复锻炼恢复大部分左上肢的功能,但手术费用较高,术后存在脱位、二次翻修、感染等风险。患者及家属权衡利弊后选择采取反式肩关节置换治疗。经入院完善相关术前准备,对该患者采取反式肩关节置换手术治疗。
全麻下,患者取沙滩椅位,左肩置于手术床外。取标准三角肌、胸大肌肌间隙入路,术中始终注意保护三角肌止点及腋神经,逐层分离至骨性结构,术中见肱骨大、小结节结构消失,骨折部位以纤维骨痂填充为主,肱骨大结节无冈上肌止点附着,冈上肌肌腱挛缩明显,残存的冈下肌、肩胛下肌及小圆肌被纤维骨痂覆盖(图1h)。肱骨头坏死吸收,术中予清除骨折部位纤维骨痂及残余坏死肱骨头,仔细分离保护冈下肌、肩胛下肌及小圆肌残存组织,充分显露肩胛盂,切除残余盂唇后显露骨性关节盂。术中使用Zimmer公司BiglianⅠ型反式肩关节假体。肩胛盂侧基座定位于肩胛盂正心位,下倾约10°(图1i)。分别用电动骨锉、髓腔挫打磨处理肩胛盂及肱骨髓腔后置入肩胛盂基座、盂侧半球形假体及肱骨柄假体试模,通过调节高分子聚乙烯杯试模高度检查三角肌张力及假体稳定性,最终确定假体型号。置入肩胛盂假体基座后2枚固定螺钉分别打向喙突基底和肩胛冈方向以牢固固定基座(图1j)。肱骨髓腔内置入骨水泥及肱骨侧假体(L=130mm,φ=10mm),并保持后倾角20°,将肩胛盂侧半球形假体(φ=36mm)安放入基座,后置入高分子聚乙烯杯衬垫(6mm)并复位关节(图1k)。由于冈上肌肌腱挛缩并脂肪化明显,术中无法修复,将残存的冈下肌、肩胛下肌及小圆肌组织以肌腱线紧缩缝合在肱骨假体柄颈部,复位关节后再次检查三角肌张力及假体稳定性,冲洗后放置负压引流,逐层关闭切口。术中出血约900ml,自体血回输500ml。
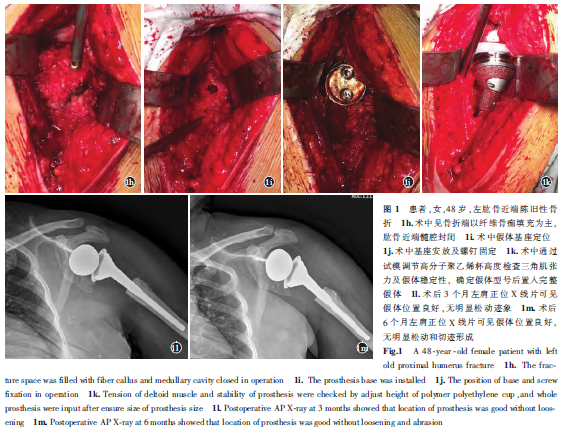
患者术后24h拔除引流管后即开始功能锻炼,术后第1周主要进行Codman钟摆运动、辅助关节功能锻炼;第2周开始进行侧卧位主动活动,轻度手法抗阻等上肢力量锻炼,术后2周常规拆线出院。术后6个月随访结果显示:患者左肩关节活动度前屈130°,外展110°,后伸40°。左侧三角肌肌力Ⅳ;术后3、6个月随访X线片(图1l,1m)示假体无脱位及松动迹象。
讨论
本例患者3年前因外伤致肱骨近端粉碎性骨折未及时手术治疗,伤后骨折端的不稳定、异常活动及血供破坏导致伤侧肱骨头坏死,逐渐形成肱骨头吸收缺如。肱骨近端骨折是老年人常见骨折类型,对于肱骨近端骨折移位较小者,通过保守治疗可达到理想的效果,但对于移位较大或粉碎性骨折应早期积极手术治疗。对于肱骨近端移位明显的粉碎性骨折,若不及时有效治疗易导致肱骨头坏死,严重降低老年人的生活质量。国内研究表明,对于NeerⅢ-Ⅳ型肱骨近端骨折,术后肱骨头缺血坏死发生率约为13%~34%。对于NeerⅢ-Ⅳ型肱骨近端骨折,若不予复位内固定治疗则肱骨头坏死率更高,在Leyshon等的研究中,3部分骨折保守治疗的肱骨头坏死发生率为29.4%,4部分骨折肱骨头坏死的发生率高达75%。随着生活条件和医疗技术的提高,伴肱骨头坏死吸收的陈旧肱骨近端骨折病例临床少有报道,但其治疗仍是棘手的临床难题。
该患者左肩CT及三维重建显示左肱骨近端大小结节结构消失,术中见骨折部位仅以大量纤维骨痂填充,肱骨近端骨缺损明显,大小结节难以重建。且左肩关节MRI显示左侧肩袖大部分缺损,冈上肌肌腱挛缩,肩袖修复可能性较小。综合分析该患者的病例特点,若选择半肩关节置换或单纯的钢板内固定治疗,由于无法修复肩袖损伤,术后的功能恢复预计难以让人满意。当肱骨近端骨缺损较大,大小结节无法重建,且合并无法修复的肩袖损伤时,反式肩关节置换成为其较理想的治疗方式。反式肩关节是指球形关节面位于肩胛盂侧,而臼杯位于肱骨近端的半限制性人工肩关节。反式肩关节具备2大设计优势:(1)反式肩关节球形假体呈1/3球形并直接安置于肩胛盂侧,使肩关节旋转中心内移,通过旋转中心内移使三角肌作用力臂增加,内移后的旋转中心位于肩胛盂表面,减少了作用在基座与肩胛盂间的剪切力,降低了肩胛盂假体松动的发生率。(2)与正常的130°左右肱骨颈干角相比,经截骨后反式肩关节的颈干角达到155°,从而使肱骨干下移。肱骨干的下移可使三角肌张力增高,且使更多的三角肌纤维参与肩关节的外展和前举运动。这些因素综合作用可最大限度发挥三角肌的动力性作用,可部分代替肩袖的功能。姜春岩等研究表明全反式肩关节置换术治疗复杂肱骨近端骨折可获得良好的临床疗效。本例患者左肩CT及三维重建显示左肱骨近端大小结节结构消失,肱骨近端骨缺损明显,但左侧肩胛盂形态基本完好,可满足反式肩关节肩胛盂侧假体基座的承载。左肩关节MRI显示左侧肩袖大部分缺损,左肩关节功能基本丧失,但左侧三角肌肌力基本正常,符合反式肩关节置换的手术指征。
值得注意的是,由于反式肩关节反解剖结构的假体设计,其术后仍存在较多并发症,术前应充分告知患者及家属此种手术的风险。其术后并发症包括:术后假体张力过低导致肩关节习惯性脱位、假体张力过大导致假体冲撞肩峰及肩胛颈、聚乙烯杯磨损、假体松动、假体周围感染等,其并发症发生率约为26.2%。其中假体周围感染被视为肩关节置换“灾难性”的并发症,并且其感染与膝关节、髋关节置换的术后感染在微生物学上存在一定的差异。研究表明,在肩关节置换手术中,有56%的肩部感染被证实是由痤疮丙酸杆菌感染引起。痤疮丙酸杆菌是一种低毒性厌氧革兰氏阳性菌,主要存在于人体上半身的皮肤,包括头部、肩部及腋窝,可通过分泌细胞毒性物质和酶来降解周围肌腱和关节囊,长期感染可导致关节脱位、假体松动。由于属于人体皮肤共存菌,其诊断存在一定困难,感染患者经常表现为各项感染相关化验指标均为正常,且肩关节穿刺液培养也难以获得细菌。但近来研究发现,由于痤疮丙酸杆菌可在假体表面形成生物膜并黏附在假体周围形成明显的滑膜炎表现,肩关节镜直视下的组织活检被认为是诊断和确定该致病菌的可靠方法。肩关节置换术后的感染,单纯的手术清创常无法完全消除感染,通常需要取出假体、彻底清创、植入含抗生素的骨水泥假体并旷置6周,期间持续静脉内使用敏感抗生素治疗后才可考虑行Ⅱ期翻修手术。
由于反式肩关节依赖三角肌提供关节的稳定性和外展动力,所以术中对三角肌张力的调控至关重要。如果关节置换术后三角肌张力过高会使假体不断撞击肩峰导致肩峰或肩胛冈骨折,如果三角肌张力过低则无法获得代替肩袖的作用力,甚至产生肩关节置换术后的不稳定。而目前三角肌张力的调节只能依靠医师的临床经验,有以下几点可供参考:术中复位关节时应有紧张感,复位后检查联合腱的张力,如果联合腱的张力紧似“琴弦”状,则往往意味着三角肌张力适当;另外,也可以通过比较双侧肢体的长度,如果双侧等长则意味患侧三角肌张力偏低,应使患侧肢体适当延长1.5CM为宜,但最长不宜超过3CM,以免术后患肢出现神经血管牵拉症状。最后,由于反式肩关节假体的无领设计及术中肩关节囊的切除,在手术时应尽量修复残存的肩胛下肌、小圆肌及盂肱韧带,且置入假体基座后2枚固定螺钉尽量打向喙突基底和肩胛冈方向以牢固固定基座,可减少基座后期松动的发生率,有助于假体的长期稳定性。反式肩关节运用于临床仅十几年时间,虽然近期临床效果满意,但中远期临床疗效仍然在随访观察中。临床通常将其视为一种最终补救措施,一旦手术失败,其翻修手术变得更加困难。反式肩关节的翻修存在骨量不足、肌肉功能不全、二次手术更易感染等问题,翻修术后的疗效更难以确定。故在选择使用反式肩关节置换时应严格把握其适应证,对于年龄<70岁的患者采用此种手术方式更需慎重。本例患者鉴于有先天性脊柱侧弯病史,既往体质一般,平时并无重体力劳动,在详细告知患者手术利弊后,患者同意接受手术并愿意承担后期高额的治疗费用,方才取反式全肩关节置换治疗。该患者近期治疗效果满意,其中远期临床疗效还有待进一步随访观察。
原始出处;
谢尚举,曹国平,全仁夫,汪灿峰.反式肩关节置换治疗陈旧性肱骨近端骨折伴肱骨头缺如1例[J].中国骨伤,2019,32(08):746-749.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#骨头#
68
#置换治疗#
75
#置换#
53
#肩关节置换#
87
#肩关节#
68
#肱骨#
67
#陈旧性#
62
#近端#
70