Neuromodulation:一项前瞻性、多中心研究,评估经舌神经刺激加物理疗法治疗轻度至中度创伤性脑损伤引起的慢性平衡缺陷的安全性和有效性
2022-01-15 MedSci原创 MedSci原创
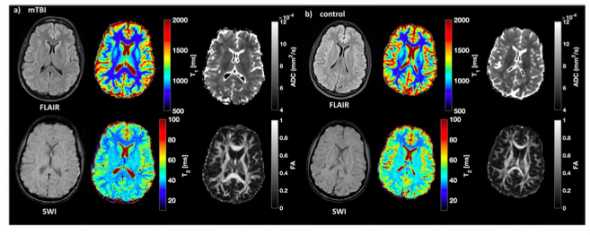
创伤性脑损伤 (TBI) 的严重程度在临床上分为轻度、中度或重度,传统上基于急性意识改变的临床测量和影像学发现。本研究使用了国防部/退伍军人管理局对 TBI 严重程度的定义。轻度至中度 TBI (mm
创伤性脑损伤 (TBI) 的严重程度在临床上分为轻度、中度或重度,传统上基于急性意识改变的临床测量和影像学发现。本研究使用了国防部/退伍军人管理局对 TBI 严重程度的定义。轻度至中度 TBI (mmTBI) 的发病率占全球 TBI 的绝大部分 (>80%),通常轻度和中度损伤的结局都比重度 TBI;然而,近四分之一的轻度 TBI 患者有持续的脑震荡后症状。包括认知、躯体和情绪问题在内的症状可能会在受伤后持续 ≥1 年,干扰日常活动并导致残疾、工作场所生产力下降,并对个人和社会造成重大负担。目前针对 mmTBI 后平衡障碍的治疗选择有限。全球约有 1460 万人在 mmTBI 后患有慢性平衡缺陷,强调了这一患者群体的未满足需求。传统治疗涉及物理治疗 (PT),通常基于前庭。对这种方法的评估表明,它可以使许多(但不是全部)患者完全康复(即恢复正常平衡和步态功能);因此,需要进行对照研究以得出关于最佳治疗的明确结论 。
经舌神经刺激 (TLNS) 是一种非侵入性方法,用于通过舌头前三分之一刺激颅神经来引发神经变化。舌头是一种理想的刺激器官,因为它具有高度神经支配,提供具有恒定 pH 值和温度的环境,并且具有低兴奋性阈值。 TLNS 向距离舌头表面约 300–400 μm 的感觉纤维提供有序的电刺激模式,以通过多个现有的突触连接产生动作电位 。这种刺激通过激活三叉神经的舌支(颅神经 Vc)和面神经的鼓索支(颅神经 VII),通过自然发生的神经网络产生信号流 。虽然鼓索的主要功能是传递有关味觉的信息 ,但颅神经和其他神经有相当多的混合,这可以为鼓索激活提供机会,同时刺激面部或其他神经分支(例如,三叉神经)。 Frehlick 等人使用高密度脑电图。据报道,TLNS 显着改变了静息状态的大脑活动。此外,高分辨率图像处理允许观察脑干、脑桥和小脑的功能活动变化,它们是大脑的主要感觉整合和运动控制中心。总之,这些数据有助于解释神经刺激的生理机制、潜在的神经变化以及可能观察到的任何临床效应之间的潜在联系。为了研究 TLNS 加 PT 在明确的同质 mmTBI 患者群体中的作用目标是评估 TLNS 加靶向 PT 对 mmTBI 后慢性平衡缺陷患者的安全性和有效性,这些患者在先前的常规 PT 计划中达到稳定状态。文章发表在《Neuromodulation: Technology at the Neural Interface》。
这项国际、多中心、随机研究招募了 122 名患有慢性平衡缺陷的参与者,他们在 mmTBI 后接受了 PT,并且恢复稳定。 随机参与者接受 PT 加高频脉冲 (HFP; n = 59) 或低频脉冲 (LFP; n = 63) TLNS。 主要疗效和安全性终点分别是感觉组织测试 (SOT) 反应者的比例(SOT 综合评分提高≥15 分)和治疗五周后的跌倒频率。治疗计划包括使用 TLNS 设备进行为期 5 周的训练,每次 20 分钟,每天 100-120 分钟,分两个阶段。第 1 阶段是为期两周的诊所培训,在此期间,参与者与获得该设备使用认证的治疗师一起工作:每天两次,每次一小时,以执行不同的培训模块(两种平衡、两种步态、一种温暖上,一次运动控制练习,一次呼吸和意识训练 [BAT]),然后是在家中独立完成的 BAT 课程。在第 2 阶段执行相同的方案,但不包括早上的 BAT 会议。第 2 阶段是为期三周的在家培训计划,参与者返回诊所进行每周监督培训,在此期间调整 PT 计划。参与者在基线和两周和五周后接受评估。所有参与者都遵循相同的 TLNS 使用和 PT 方案;训练强度是根据个人的表现和能力定制的。通过 TLNS 设备通过记录使用情况自动监控依从性;这些数据每周下载和验证,并确定合规率。
与基线相比,HFP + PT (71.2%) 和 LFP + PT (63.5%) 组的 SOT 反应者比例显着(p < 0.0005)。 对于汇总人群,SOT 反应率为 67.2%(p < 0.00005),并且在两周和五周后,SOT 综合评分在临床和统计学上都有显着改善(p < 0.0005)。 两组的跌倒和头痛残疾指数评分均有所降低。 在第 2 周和第 5 周,两组的平均动态步态指数评分也较基线显着增加。这项研究是针对 mmTBI 后慢性平衡缺陷患者进行的最大的多中心随机试验,这些患者在之前的康复计划中处于稳定状态。这项研究的结果表明,TLNS 加靶向 PT 与 HFP 或 LFP 刺激在该人群中具有显着的益处。两组的 SOT 综合评分和 DGI 较基线的改善具有统计学意义和临床意义,分别定义为 SOT 综合评分至少增加 8 分和 DGI 评分至少增加 2.9 分。本研究中的响应者分析使用 15 分作为截止阈值来证明 SOT 的改善,几乎是已证明具有临床意义的变化的两倍。
除了头痛、睡眠质量和跌倒频率外,TLNS 加靶向 PT 还观察到平衡和步态的显着改善; 在 mmTBI 后出现慢性平衡缺陷并且在之前的常规物理治疗中处于稳定状态的参与者中。
Ptito, A., Papa, L., Gregory, K., Folmer, R.L., Walker, W.C., Prabhakaran, V., Wardini, R., Skinner, K. and Yochelson, M. (2021), A Prospective, Multicenter Study to Assess the Safety and Efficacy of Translingual Neurostimulation Plus Physical Therapy for the Treatment of a Chronic Balance Deficit Due to Mild-to-Moderate Traumatic Brain Injury. Neuromodulation: Technology at the Neural Interface, 24: 1412-1421. https://doi.org/10.1111/ner.13159
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#前瞻性#
64
#多中心#
52
#安全性和有效性#
56
#创伤性#
75
#多中心研究#
0
#创伤#
55
#神经刺激#
69
#损伤#
54
#物理疗法#
72