J Thorac Oncol: 小细胞肺癌(SCLC)预防颅内照射避免或不避免海马结构(HA)的疗效:随机III临床试验(NCT01780675)
2021-05-15 yd2015 MedSci原创
小细胞肺癌(SCLC)预防颅内照射没有避免海马照射(HA-PCI)并没有导致明显神经认知功能下降,2年脑转移率也没有明显升高。
小细胞肺癌(SCLC)患者具有很高的几率出现脑转移(BM)。伴有BM的SCLC患者颅脑放疗可以改善生活质量。而预防性颅脑照射(PCI)可以很大程度预防BM的发生。有研究表明预防颅内照射避免或不避免避免海马结构(HA)对神经认知功能改变有明显差异。但是,对长期的认知功能影响尚未得知。
因此,国外学者进行了相关研究,并在Journal of Thoracic Oncology杂志发表了相关研究成果。该研究是多中心、随机III临床试验(NCT01780675)。纳入患者分为预防颅内照射避免海马照射(PCI)和预防颅内照射没有避免海马照射(HA-PCI)。纳入标准:组织学或细胞学诊断的I-III期或IV期的SCLC,没有脑转移瘤,同时I-III期SCLC放化疗后以及IV期患者化疗后无进展。年龄小于18岁,既往接受过PCI的患者被排除。最后一次化疗时间距离PCI需要间隔至少3周。患者予25 Gy/10次。检测基线、PCI后第4,8,12,18和24小时的神经认知功能。主要终点为第4个月时霍普金斯语言学习测试修订版(HVLT-R)的全面回忆;比基线至少下降了5个百分点被认定是失败。次要终点包括其他认知结果,发病率评估,脑转移的位置和总生存率。
研究纳入荷兰和比利时10个中心2013年4月至2018年3月的168例患者, PCI和HA-PCI组的患者均为84例。中位随访时间为24.8个月(23.5–32.8个月)。中位年龄为64岁。一共157例(96%)接受25 Gy/10次治疗。
主要研究终点达到时共102例患者纳入分析,其中PCI组46例患者,HA-PCI 组为56例。总体人群中,29 (28%)例患者出现大于等于5% HVLT-R的全面回忆的下降。在PCI组中为29%,而HA-PCI组为28%,两组没有统计学差异(p=1.000)。在其他认知测试中,测量记忆,执行功能,注意力,运动功能和处理速度在两组中没有明显差异。

两组的临床特征
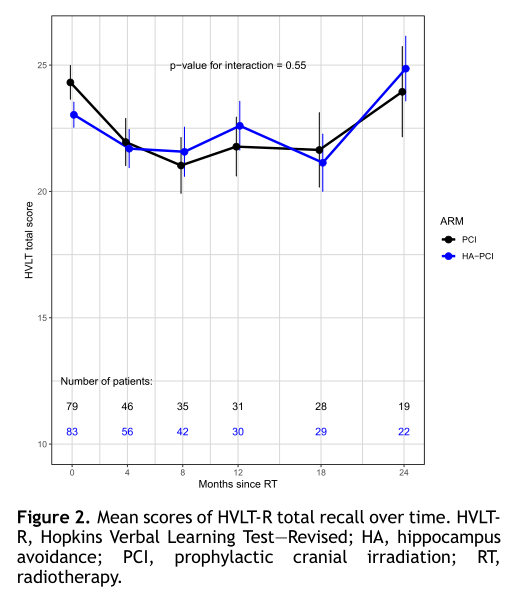
两组HVLT-R率
2年累计脑转移率:PCI组为20%(95%CI:12%–29%),而HA-PCI 组为16%(95%CI: 7%–24%) 。发生脑转移的31例患者中,74%为多发性。13例患者无症状,16例患者有症状,其他2例情况不明。
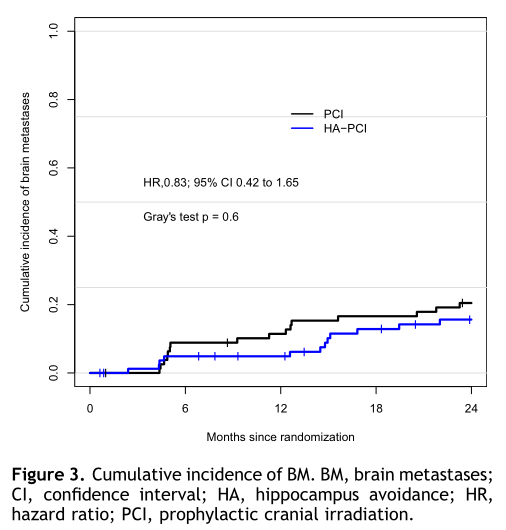
两组脑转移发生率
截止数据时,168例患者中有102例死亡(HA-PCI组49例和PCI组53例)。HA-PCI 和 PCI 组的中位OS为18.5和19.9个月(HR=0.93, 95% CI: 0.63–1.37),两组OS没有明显统计学差异(p=0.70)。亚组分析发现,I-III期对比IV期患者的OS在两组中也没有统计学差异。
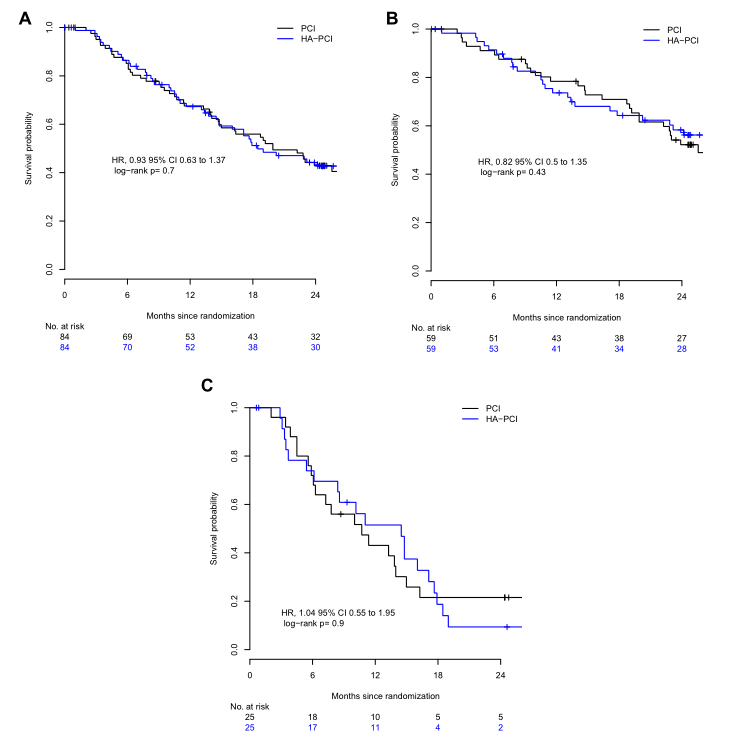
中位OS的比较
综上,小细胞肺癌(SCLC)预防颅内照射没有避免海马照射(HA-PCI)并没有导致明显神经认知功能下降,2年脑转移率也没有明显升高。
原始出处:
José S A Belderbos, Dirk K M De Ruysscher, Katrien De Jaeger, et al. Phase 3 Randomized Trial of Prophylactic Cranial Irradiation With or Without Hippocampus Avoidance in SCLC (NCT01780675). J Thorac Oncol. 2021 May;16(5):840-849. doi: 10.1016/j.jtho.2020.12.024.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#THORAC#
70
#Oncol#
87
#III#
70
谢谢梅斯提供这么好的信息,学到很多
86
JTO上有很多不错的好文章,谢谢梅斯及时上新
112
谢谢梅斯分享这么多精彩信息
104
高质量研究,读起来真爽,谢谢梅斯
0